Men less likely to specialize in mammography, calling it ‘female-only’ work
Male medical students exploring specialization options are less likely to opt for mammography over other imaging modalities, citing discrimination and fear of sexual harassment suits as drawbacks, according to research out of Callaghan, Australia.
Despite the high incidence of breast cancer across the country, author Helen M. Warren-Forward, PhD, said in Radiography this month, Australia is suffering from a lack of interest in the field. A 2009 study found the average age of radiographers in mammography was a decade older than their counterparts in CT and MRI, and 30 percent of that workforce was already expected to retire within five years.
“The Evaluation of the BSA Programme team projected that demand for screening will outweigh capacity by 2014,” Warren-Foward, an associate professor in the School of Health Sciences at the University of Newcastle, said. “This has not become a reality, however there is a major issue recruiting radiographers to breast screening.”
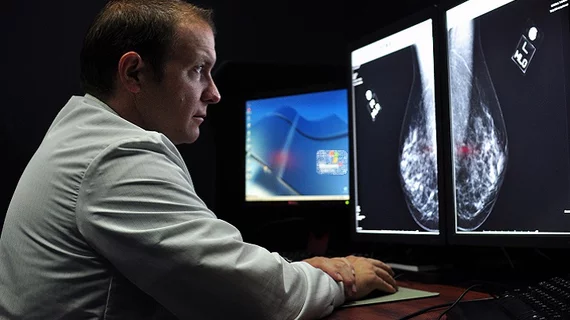
A noticeable gender divide exists in the field, too, she wrote. Breast imaging in Australia is currently only conducted by female radiographers, but practices short on imaging experts are considering opening their doors to qualified men, too.
“A number of authors have researched mammography client perceptions to being examined by a male radiographer and preliminary research has indicated that a mix of male and female radiographers would be accomodated,” Warren-Forward wrote. “However, it is uncertain if male radiographers would be interested in undertaking this role.”
To assess that, Warren-Forward distributed a survey to 248 undergrads enrolled in the Bachelor of Medical Radiation Science program at the University of Newcastle, asking them to detail their experiences with six imaging modalities and rank them by interest and what they’d like to specialize in.
Just over 100 students replied to the survey, according to the study, and the whole pool indicated they’d been taught all six modalities, including angiography, CT, fluoroscopy, MRI, mammography and ultrasound, even if they hadn’t experienced them in clinical practice yet. Ultrasound, CT and fluoroscopy were the most commonly known modalities, with 90 percent, 97 percent and 80 percent of students, respectively, indicating they’d either observed or performed the procedure.
In comparison to ultrasound, CT and MRI—the most popular modalities for specialization across the board—few students had experience in mammography, Warren-Forward said. Seventy-seven percent wrote they’d be uncomfortable performing mammograms, with five times more men than women agreeing with the statement. Around half of each gender said they felt the procedure was inappropriate, while 58 percent of males said “fear of being sued for inappropriate sexual harassment” was a main drawback. Ninety-two percent of men said they didn’t want to pursue mammography simply “because I am male,” calling the specialization “female-only” work and reporting feeling unwelcome in the field.
“Students have limited access to mammography, and this seems to be a major factor into why radiographers do not choose mammography as a specialty,” Warren-Forward wrote. “Increasing academic curricula and accessibility during clinical placement may aid in the perception of mammography among radiographers.”
Students said role extension possibilities and better pay would also be successful incentives for drawing more young professionals to the field, and Warren-Forward said women might be more likely to stay in mammography if they did the work part-time, alongside rotations in different modalities, to avoid repetition and burnout. Finally, she said, the specialization needs to think about gender inclusivity.
“The gender divide may have to be bridged to enable crucial recruitment, as male students feel discriminated against,” she wrote.