DBT associated with more accurate biopsy recommendations
Digital breast tomosynthesis (DBT) implementation in a diagnostic setting can result in an improved cancer detection rate (CDR) and more accurate biopsy recommendations, according to a new case study published in the Journal of the American College of Radiology.
“Although DBT may better characterize malignant and benign features, and therefore have the potential to decrease unnecessary imaging follow-up and ultimately benign biopsies, the current literature is inconsistent,” wrote Emily B. Ambinder, MD, of Johns Hopkins Medical Institutions in Baltimore, Maryland, and colleagues. “Therefore, we aimed to add to this important topic by assessing the impact of DBT on outcomes in the diagnostic setting.”
The researchers studied more than 23,000 diagnostic mammographic studies performed from July 1, 2013 to June 30, 2017, at four breast imaging locations belonging to a single institution. DBT was implemented at these locations through those four years, and data was separated into two groups: a full-field digital mammography (FFDM) group, which included studies performed before DBT implementation, and a DBT group, which included studies performed at least one year after DBT implementation.
The study included more than 5,700 examinations from the FFDM group and more than 9,700 examinations from DBT group. Overall, 71.1 percent of examinations from the FFDM group had a BI-RADS 1 or 2 assessment. That number was 73.7 percent for the DBT group. Also, 15.3 percent of examinations from the FFDM group had a BI-RADS 3 assessment, higher than the DBT group’s 12.9 percent. These statistics are important, the authors noted, because of what fewer BI-RADS 3 assessments can mean for both patients and healthcare providers.
“The original goal of the BI-RADS 3 category was to safely reduce the number of biopsies that would likely lead to benign outcomes on pathologic analysis,” the authors wrote. “Use of the BI-RADS 3 category undoubtedly leads to patient anxiety and increased health care utilization and cost.”
In addition, the FFDM group had a cancer detection rate of 28.9 and a positive predictive value from biopsy recommendation (PPV2) of 21.3. The DBT group had a CDR of 45.4 and PPV2 of 34.0.
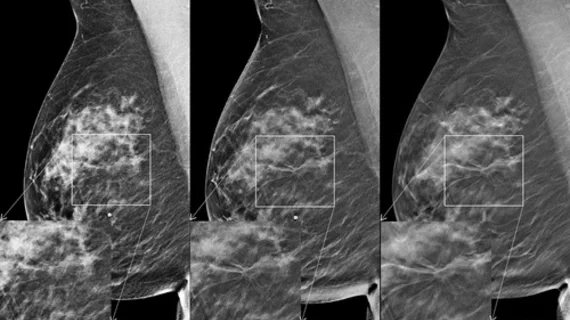
“This suggests improved accuracy in the assessment of lesions recommended for biopsy, increasing the number of cancers biopsied and decreasing false-positive results,” the authors wrote. “Prior studies with similar results suggested that the improved metrics could be due to the ability of DBT to offer a more comprehensive evaluation of lesions by providing improved visualization of margin features, having lower structure noise from normal surrounding breast tissue, and detecting additional findings obscured when only FFDM is used, all of which could lead to a more accurate diagnosis.”
The team did note that their study was limited by only tracking results from a single institution, “so its results may not be generalizable to other clinical settings.”