American Society of Nuclear Cardiology urges Congress to speed prior authorizations, repeal AUC mandate
The American Society of Nuclear Cardiology (ASNC) is lobbying Congressional leaders to take action on prior authorization and call for the repeal of the Medicare Appropriate Use Criteria (AUC) mandate.
Over the past few weeks, members of ASNC’s Health Policy Committee have held meetings with their members of Congress. One of the key messages to Congress has focused on requesting co-sponsorship of the Improving Seniors’ Timely Access to Care Act (S. 3018 and H.R. 3173). The bill is aimed at protecting seniors citizens from delays and interruptions in care that result from the prior authorization process in the Medicare Advantage (MA) program.
The legislation would require electronic prior authorization, improve transparency for beneficiaries and providers, and increase oversight from the Centers for Medicare and Medicaid Services (CMS) on how MA plans use prior authorization. The ASNC said the act recognizes that physicians should be focused on patient care, not on navigating the prior authorization process to get patients their recommended tests, procedures and treatments.
The ASNC said this legislation has strong bipartisan support, including more than half of the House of Representatives. ASNC is encouraging lawmakers who are already cosponsors to ask for committee action on the legislation this year, which would create a path for final passage.
"It's not the appropriate use criteria we have an issue with, its the decision support mandate, because it is overly prescriptive and there is a hassle factor and a time factor involved," explained Randall Thompson, MD, immediate past ASNC president, attending cardiologist at St Luke's Mid-American Heart Institute, and professor of medicine, University of Missouri, Kansas City School of Medicine.
Thompson said the mandate would take away resources from efforts in quality improvement by requiring additional administrative burden. "This is at a time when most of us are struggling with staffing just like the rest of the economy is," he said.
The PACS and cardiovascular information system (CVIS) vendors also have had issues with the mandate. Part of it was that there was a lack of a final rule guidnance from CMS on how an AUC system needs to operate to be approved, so nothing could be programmed. Then there is the need to constantly update the software in a timely manner as guidelines and expert consensus recommendations change on a regular basis. Medical societies have concerns this could cause issues when doctors order a test and the software tells them no because it has not yet been updated. There are also fears among physicians that less sophisticated software might be adopted by health systems because they are easier to interface with an electronic medical record (EMR) system, or are less expensive but also come with less functionality.
"My hospital decided to use something that was less expensive, embedded it into the electronic medical record, but it is totally different and there are discrepancies between the systems' appropriate use criteria and one ones that I am using," Thompson said.
ASNC calls on Congress to repeal the appropriate use criteria mandate
ASNC's Health Policy Committee members continue to push for the repeal of §218 of the Protecting Access to Medicare Act (PAMA), which mandates the use of prescribed clinical decision support mechanisms to consult AUC when ordering any advanced diagnostic test.
"ASNC is and always has been an ardent supporter and developer of AUC, but objects to the inflexibility and complexity of the program," the ASNC’s Health Policy Committee said in a statement. The committee said AUC as it is currently set up, does not fit into physician workflow. The ASNC believes the AUC mandate program adds administrative burdens on providers that add extra cost to healthcare, and disproportionate cause burdens for medical imaging utilization.
The ASNC part of a coalition of more than 30 medical societies asking Congress to repeal the program.
Details of the Medicare AUC requirement
Section 218 of PAMA states, "Prescribes quality incentives to promote patient safety and health, including penalties, for certain computed tomography services. Directs the Secretary through rulemaking to specify appropriate use criteria (AUC) for imaging services only from those developed or endorsed by national professional medical specialty societies or other provider-led entities. Requires the Secretary then to promote the application of such criteria by ordering professionals and furnishing professionals to imaging services furnished in a physician's office, a hospital outpatient department (including an emergency department), an ambulatory surgical center, and any other provider-led outpatient setting."
In 2014, Congress passed PAMA, establishing the Medicare Appropriate Use Criteria (AUC) Program for advanced diagnostic imaging. It mandates providers used AUC decision support tools to justify the use of advanced medical imaging. The ASNC said in its statement that nearly eight years later, the AUC program implementation and rule making are still incomplete. This has prompted concerns about the law’s complexity and the cost and regulatory burden incurred by physicians and other healthcare providers to meet program requirements if the program were ever to take effect, in whole or in part.
Through their medical societies and institutions, physicians have led the way with the development of AUC for diagnostic imaging, and they continue to advocate for its use. Independent, evidence-based guidelines are also widely used throughout the healthcare system, including for advanced imaging.
"Although Congress may have believed the AUC Program was a straight forward approach to encourage the use of AUC by clinicians who order advanced imaging tests, the law has always faced implementation challenges and opposition from physicians who are weary of the imposition of new administrative burdens of questionable value. In some cases, the law would actually preclude utilization of well-established physician guidelines," the ASNC Health Policy Committee wrote.
Since PAMA’s enactment, new Medicare payment and delivery models that hold clinicians accountable for healthcare resource use have evolved.
"When coupled with repeated implementation delays, the AUC Program is now outdated. It should be repealed, and Medicare should leverage existing quality improvement programs to encourage the consultation of AUC for advanced diagnostic imaging," the ASNC said.
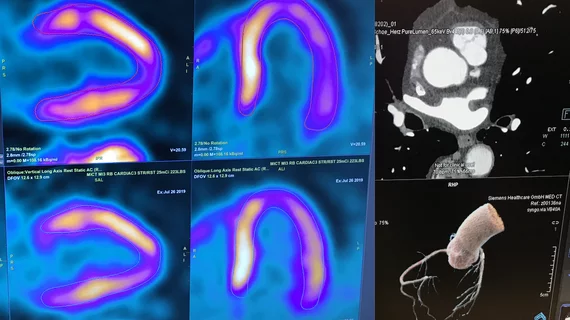
Under PAMA, advanced imaging services include:
• Computed tomography (CT);
• Positron emission tomography (PET);
• Nuclear medicine; and
• Magnetic resonance imaging (MRI).
If ever fully implemented, the AUC Program would apply to every clinician who orders or furnishes an advanced diagnostic imaging test, except for emergency and inpatient services. CMS has acknowledged the number of clinicians affected by the program is “massive,” crossing almost every medical specialty and having a particular impact on primary care physicians since their scope of practice can be vast.
The law is very prescriptive, requiring consultation of AUC using a qualified Clinical Decision Support Mechanism (CDSM) at the time a practitioner (or clinical staff acting under a practitioner’s direction) orders an advanced diagnostic imaging service for a Medicare beneficiary. The CDSM provides a determination of whether the order adheres to AUC or if the AUC consulted was not applicable.
Upon consulting AUC, the ordering professional must provide information to furnishing professionals and facilities, who must, in turn, report this AUC consultation information on their Medicare claims to be paid for the test. This information includes the ordering professional’s National Provider Identifier (NPI), the CDSM consulted, and whether the service ordered will adhere to consulted AUC, or whether consulted AUC was not applicable to the service ordered.
The ASNC and other medical imaging societies said this ultimately will lead to practitioners whose ordering patterns are considered outliers to be subjected to prior authorization.
The law established 2017 as the program’s start date. However, technical challenges have impeded implementation. The program’s penalty phase will now occur on or after Jan. 1, 2023, or the January 1 that follows the declared end of the public health emergency for COVID-19.
However, the ASNC said there is no indication CMS can even implement the AUC Program in a manner that fully complies with the law due to challenges with operationalizing documentation requirements on Medicare claims. For this reason, the ASNC is requesting lawmakers repeal the AUC Program.
Changes in healthcare delivery models has made the AUC Program outdated
Beyond implementation challenges since its enactment, the ASNC said the AUC Program has become outdated. This is mainly due to the subsequent enactment of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) and the rise of new healthcare payment and delivery models. These newer payment models hold clinicians responsible for healthcare resource use, such as alternative payment models and the Merit-based Incentive Payment System (MIPS) and Primary Cares Initiative.
For example, on November 20, 2020, the Center for Medicaid and Medicaid Innovation announced details of the first cohort of Primary Care First participants, which includes 916 primary care practices. Primary Care First, which began on January 1, 2021, will focus on advanced primary care practices ready to assume financial risk by moving away from fee for service to a prospective population-based payment. Under such a payment arrangement, primary care physicians will be incentivized to improve quality and patient experience of care and reduce expenditures through appropriate utilization of healthcare resources.
By finalizing new exceptions to the physician self-referral law for value-based arrangements, CMS recognized value-based healthcare delivery and payment systems, by design, provide safeguards against over utilization.
While there may be differing ideas about how to foster the use of AUC by clinicians, there is widespread agreement the program should not and cannot be implemented as originally envisioned, the ASNC stated. The society said the AUC Program should be repealed on the basis that the program diverts provider resources away from quality improvement activities. The AUC Program implementation is occurring at the same time providers are struggling to assign adequate resources for information technology infrastructure and Quality Payment Program participation. The AUC Program has no metrics of quality or patient outcomes, the ASNC said.
There also have been universal concerns from most medical societies that struck adherence to AUC will take away provider flexibility. The prescriptive nature of the law and accompanying rules will, in many cases, force clinicians to abandon long-standing methods of AUC consultation, as well as the consultation of specialty-specific AUC and guidelines, the ASNC said.
There are also concerns that requiring recording of AUC documentation adds administrative burden and adds to health IT issues where the complex exchange of information between clinicians and software is not yet supported by interoperable electronic health record (EMR) systems and relies on claims-based reporting. At the same time, CMS is migrating away from claims reporting for quality data.
Watch the VIDEO: Imaging societies ask Congress to repeal appropriate use decision support mandate — Interview with Randall Thompson, MD, for more information.