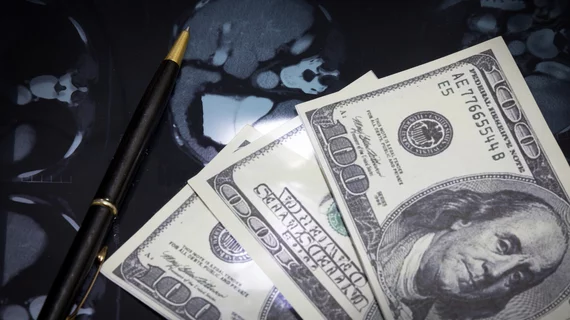
Medicare finalizes 2024 physician fee schedule with radiologist pay cuts, pause of AUC program
The Centers for Medicare & Medicaid Services on Thursday issued the final 2024 physician fee schedule, which includes radiologist pay cuts and a pause of the imaging Appropriate Use Criteria program.
CMS has finalized a 2024 conversion factor (the dollar amount used to convert RVUs into payment) of $32.74, a 3.4% (or $1.15) decrease from last year. Absent any congressional action, diagnostic radiology will face a 3% pay decrease, while interventional specialists will see an aggregate 4% decrease, versus a 3% drop for radiation oncologists, experts estimated.
The actual impact could be worse, the American College of Radiology noted, as these numbers do not account for payment changes tied to the Consolidated Appropriations Act. Physician advocacy groups including the American Medical Association, Medical Group Management Association and the American Society for Radiation Oncology criticized the final fee schedule following its release.
“Again, CMS has placed physicians and especially radiologists in a position to examine an unclear path forward as practice expenses increase and Medicare reimbursements decline,” Radiology Business Management Association Executive Director Bob Still said Thursday. “Radiologists continue to get a smaller piece of the Medicare physician pie. RBMA and other organizations will come together to work with Congress to correct the inequity in Medicare physician payments.”
Overall, CMS has reduced finalized payment amounts under the fee schedule by 1.25%, “in accordance with update factors specified by law,” the agency noted. Medicare also is moving forward with payment increases for many services, including primary and “longitudinal” care.
As first proposed in July, CMS confirmed that it is pausing implementation of the long-delayed imaging Appropriate Use Criteria program, including ending the current educational and operations testing period. First established in 2014, the initiative requires physicians to consult a decision-support system before ordering MR, CT and other advanced imaging to help curb healthcare waste. But it’s been plagued by postponements and other challenges.
The American College of Radiology, which has supported the program, acknowledged the pause while holding out hope that AUC could return in the future.
“The ACR recognizes the significant issues CMS faces with the real-time claims processing aspect of the AUC program and the potential impact on our members should claims be denied inappropriately,” ACR said in its initial analysis of the final fee schedule, issued late Thursday. “The college is working with Congress to streamline and modernize the [Protecting Access to Medicare Act’s] AUC program, including the removal of this requirement, to allow the program to move forward and ensure Medicare patients receive the right imaging tests at the right time.”
The payment schedule confirms that the Medicare Economic Index—a government measure of inflation in medical practice costs—increased at 4.6%. This would mark the highest uptick this century, the AMA noted, and is on top of a 3.8% increase last year. When adjusting for inflation, Medicare physician payment effectively declined 26% between 2001 to 2023, before including these cuts, the association noted.
“This is a recipe for financial instability. Patients and physicians will wonder why such thin gruel is being served,” AMA President Jesse M. Ehrenfeld, MD, said Thursday.
Advocates believe these numbers underline the need for legislative fixes such as the Strengthening Medicare for Patients and Providers Act. The bipartisan bill would provide a permanent annual inflationary physician payment update tied to the Medicare Economic Index.
“The AMA and house of medicine strongly urge Congress to advance this legislation,” Ehrenfeld added.
You can read more about the final fee schedule in the CMS press release, corresponding fact sheet and the 2,709-page rule itself. The policies will be effective beginning Jan. 1.