Academic and hospital-based mammography embraces teleradiology: Shedding 3 preconceptions of the past
In 2020, a growing health system in the Northeast asked vRad for assistance. Like many providers around the country, all of its hospitals were struggling with physician shortages that largely stemmed from recruiting challenges.
Mammography stood out among the enterprise’s hardest-hit medical specialties. Its subspecialized breast radiologists were perilously overstretched.
And the health system had never considered “outsourcing” mammography an acceptable option.
Their thinking was not uncommon: Surely no national telemammography team could understand the nuances of a regional health system’s practice. Equally unlikely was the notion that remote readers could uphold the high level of quality and the personal interaction that patients and referrers expect from dedicated breast care.
However, with delays mounting for screening mammograms, diagnostic exams and IR procedures, teleradiology didn’t seem so farfetched a proposition. So the decision-makers sized up potential partners, did their due diligence and decided to partner with the telemammography team I lead at vRad to augment their local radiologists.
We started by reading breast images remotely for two of their 15 campuses.
How has that worked out? Very well. A year after facing its breast-care crisis with anxious hope, the health system is expanding its vRad partnership to additional hospitals.
This experience reflects a familiar story nationwide. As hospital systems extend into their local communities, we are extremely proud to be able to help them continue providing expert care. We become part of the hospital team, delivering subspecialist image interpretation and interacting directly with patients and referrers alike.
A practical imperative
Simple arithmetic dictates that no breast radiology operation can place a subspecialist at every facility in which cancer gets treated. Despite this, many full-service medical centers embraced a go-it-alone mentality around breast imaging. Some assumed it just couldn’t be done effectively remotely.
This may be the first of the offhand assumptions that need to fall if telemammography is to help U.S. healthcare extend the reach of subspecialist breast care.
And it surely should do so. The dearth of experts demands it.
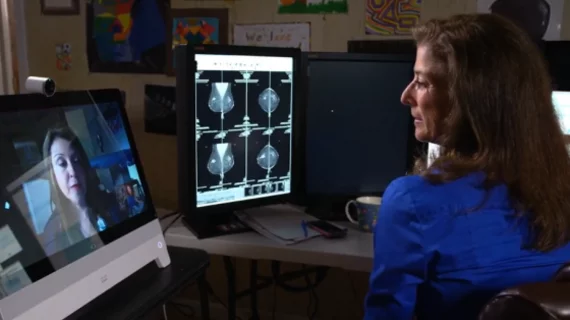
Now that images are protectable and portable through the cloud—and radiologists can speak face-to-face with patients and technologists via video phone—it’s not just possible to extend access to patients who otherwise wouldn’t have exposure to subspecialists. It’s the right thing to do.
Happily, from what I’m seeing, more and more facilities—even top academic medical centers—are coming to agree with that moral imperative.
Not everyone is warmed up to the idea yet, so let’s look at three lines of faulty thinking about telemammography that persist.
Misperception 1. To acquire and maintain high-level expertise, a breast radiologist needs to physically work inside a bricks-and-mortar environment.
- REALITY: All 13 of the radiologists on my team at vRad are fellowship-trained mammographers. We’re on the boards or otherwise meaningfully involved with the American College of Radiology and the Society for Breast Imaging.
We’re members of the same committees on which our academic peers sit. We’re in the plenary commissions that plan and discuss best practices. We’re participating members in care-improvement work at the national level. We participate in multidisciplinary tumor boards remotely.
Meanwhile, most referrers are not physically present in hospitals. They themselves are seeing their patients in an outpatient setting, and they’re receiving reports from outside specialists. Happily for patients and hospital breast departments, the sticking point over physical presence is starting to dissolve.
Misperception 2. “Teledoctors” don’t fit into on-site radiology workflows.
- REALITY: vRad’s telemammography program is specifically set up to make our breast specialists de facto members of the local team. We study their reporting and workflows before entering the hospital’s program. Their referrers get to know us, their patients get to know us, and we work just as closely with their technologists as if we were standing at their side. All of this is a snap with our high-definition videoconferencing platform.
Our clients are now able to offer same-day diagnostics and most of the diagnostics patients are getting direct interaction with the radiologist, not just BI-RADS 4 and 5 category patients.
Misperception 3. Teleradiology is like a hasty assembly line, too focused on quantity to concentrate on quality.
- REALITY: At vRad, we measure and track everything related to diagnostic accuracy. Our QC program is arguably the most rigorous in the country. Our cancer-detection rates are well within the national recommendations.
In other words, you can’t see a difference between our care and any other fellowship-trained care out there.
I’ll take this point one step further. We not only provide these metrics to our client sites but also handle MQSA compliance activities. We take care of the physicist end as well as quality control—the very things that keep hospital breast departments up at night.
Are they auditing and tracking all patients? vRad has a very sophisticated system for tracking patients. Our reports transmit through an HL7 connection to our clients’ PACS, so those communications are completely automated and totally hands-free. The results get translated into the proper, evidence-based recommendations, right into their PACS.
Those are the kinds of things that administrators and technologists worry about and we don’t. We get a great deal of satisfaction handling all these things and helping our client sites tackle them. We’re even expert at annual MQSA inspections.
Here for the long haul
vRad recently increased its radiologist roster from 10 to 13 fellowship-trained breast subspecialists. We’re likely to add more as providers get past old preconceptions and embrace excellence offered from elsewhere.
In fact, we’re starting to work closely with some leading academic institutions. As these major innovators expand their expertise into local communities, many struggle to maintain a high level of care out in their community hospitals, urban clinics and satellite sites.
Consider this. I have a lot of CVs on my desk from fellowship-trained breast radiologists. The physician shortage is real, yet vRad’s approach to telehealth is such a great model for both physicians and facilities that I have a problem of my own: trying to figure out which expert physician to interview next. vRad’s practice model works just that well.
I see it this way. Today’s hospitals and health systems have to provide excellent service to patients and referrers just as they always have. But now they have to serve their customers in a way that’s economically sound and operationally efficient.
To their credit, many have recently embraced the reality that working from home is here to stay in medicine—not only for administrators and support staff but also for clinicians.
Who’s better suited to serve under this new paradigm than diagnostic radiologists specialized in breast care?
For more on vRad telemammography, and to view an in-depth discussion led by Dr. Sussman, click here.