2022 Radiologist Job Market Update: High volume, high pay and a search for high quality of life
More than two years after the onset of the pandemic, changes in COVID-related policies and postures — as well as accompanying cultural shifts in the workplace — continue to drive trends in the job market for radiologists. In 2022, things look markedly different than during the early stages of the pandemic and it’s clear that radiologist job seekers now have many options and greater workplace flexibility.
In my role as medical director for vRad, I work very closely with our physician recruiters. Between us we interview hundreds of radiologists every year as they explore options for their next career move. This experience along with the other datapoints available from serving 2,100 imaging facilities and radiology groups nationwide give us unique insights into the radiologist job market nationally.
With the numbers in radiologists' favor, we’re seeing some other noteworthy trends: higher compensation for experienced radiologists, an uptick in retirements, and increasing demand among radiologists for more flexible, remote-friendly working options, among others.
Here, we’ll further explore the current state of the radiologist job market and look ahead to what we can reasonably expect to see in the future.
Supply and demand of radiologists
To understand today’s job market, it’s useful to look at national imaging volume levels coming out of the pandemic. In January 2021, Emergency Department visits remained below pre-pandemic levels according to the CDC. By mid-March however, ED imaging volume here at vRad was surging past our pre-pandemic baseline. In the same timeframe, stories were appearing from places around the U.S. like Oregon and Minnesota reporting a similar increase in ED traffic. Throughout the summer, imaging volume continued climbing to new highs relative to our 20 years of tracking radiology data.
Many radiology groups struggled to keep up with the sudden increase in volume and while a COVID-related bounce is largely responsible for propping up the short-term numbers, long-term trends make it clear that these higher volumes are likely the new normal.
Projections of severe physician shortages have been well publicized and the Association of American Medical Colleges (AAMC) is forecasting a 42.4% growth in the population of Medicare beneficiaries by 2034. Providers are bracing for a shortage of specialists whose work often deals with older patients. A similar story has already played out in England.
We're also starting to see signs of a possible uptick in retirements. Between 2014 and 2018, vRad’s attrition rate due to retirement was about 1% but in recent years that has risen to 2-3%. With 500 radiologists in our practice, we view those numbers as suggestive of a national trend.
Medical providers react, let the hiring begin
Leading physician staffing company Merritt Hawkins notes in its 2021 Review of Physician and Advanced Recruiting Practitioner Incentives that radiology now ranks as the third-most requested specialty, preceded only by nurse practitioners and family medicine physicians. This report represents the height of the pandemic, from April 1, 2020 to March 31, 2021, at a time when imaging volumes were still low — and even then, radiologists were in high demand.
That demand continues to increase. 2021 was a record year for job postings on the American College of Radiology (ACR) job board. The graph below visualizes that increase, with the number of new job postings dramatically rising throughout the year (see figure 1.1).
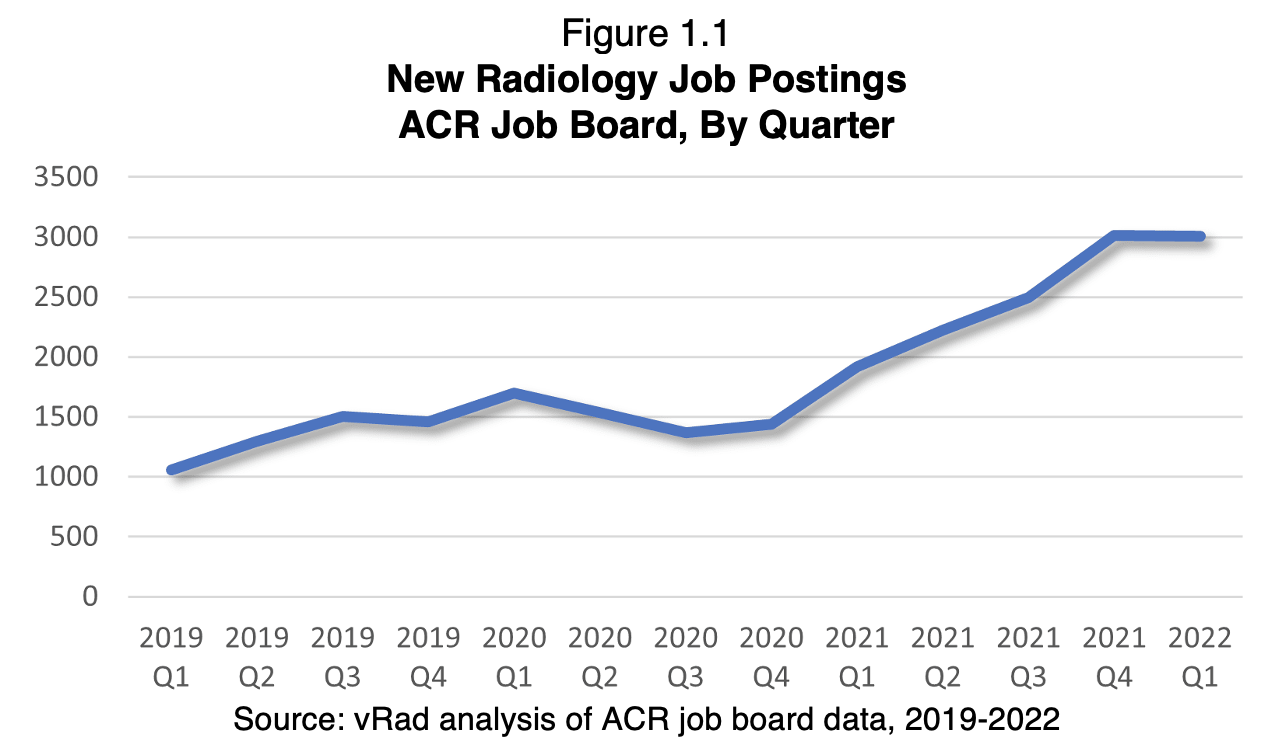
These observations and trends lead us to believe that radiologists will continue to be in high demand.
Rising compensation climbs even higher for experienced radiologists
It's no surprise that with strong demand for radiologists, compensation increases have followed. That includes high offers for new radiologists (radiologists earn the fifth highest starting salaries of all specialties) and signing bonuses of $10,000 to $50,000 according to the Merritt Hawkins report. Radiologists are also receiving “stay bonuses” and pay increases from their current employers in an effort to increase retention.
Our own practice is no exception: In October 2021, vRad announced increases in compensation for the fourth consecutive year. The increases — up to 25% — took effect this past January.
The report also suggests that experienced radiologists seem to have gained the most from the hot job market. On the “high” end of radiologist salaries, their wages jumped from an expected $577,000 to $825,000 — and that doesn’t include benefits. The year held less cause for celebration among radiologists in the “low” and “average” compensation categories, which actually saw a slight decrease in salaries between 2019-2020 and 2020-2021.
While it’s fair to say that wages are quite high and so is competition for talent, it’s also important not to hyperbolize the generally upward salary trends in the field. Many providers will be wary of extreme changes that could permanently skew expectations or start competitive “bidding wars” for talent. Our internal review of 200 ACR job postings in January 2022 showed that only 11% of jobs were indeed offering the industry-hyped signing bonuses — but 89% were not.
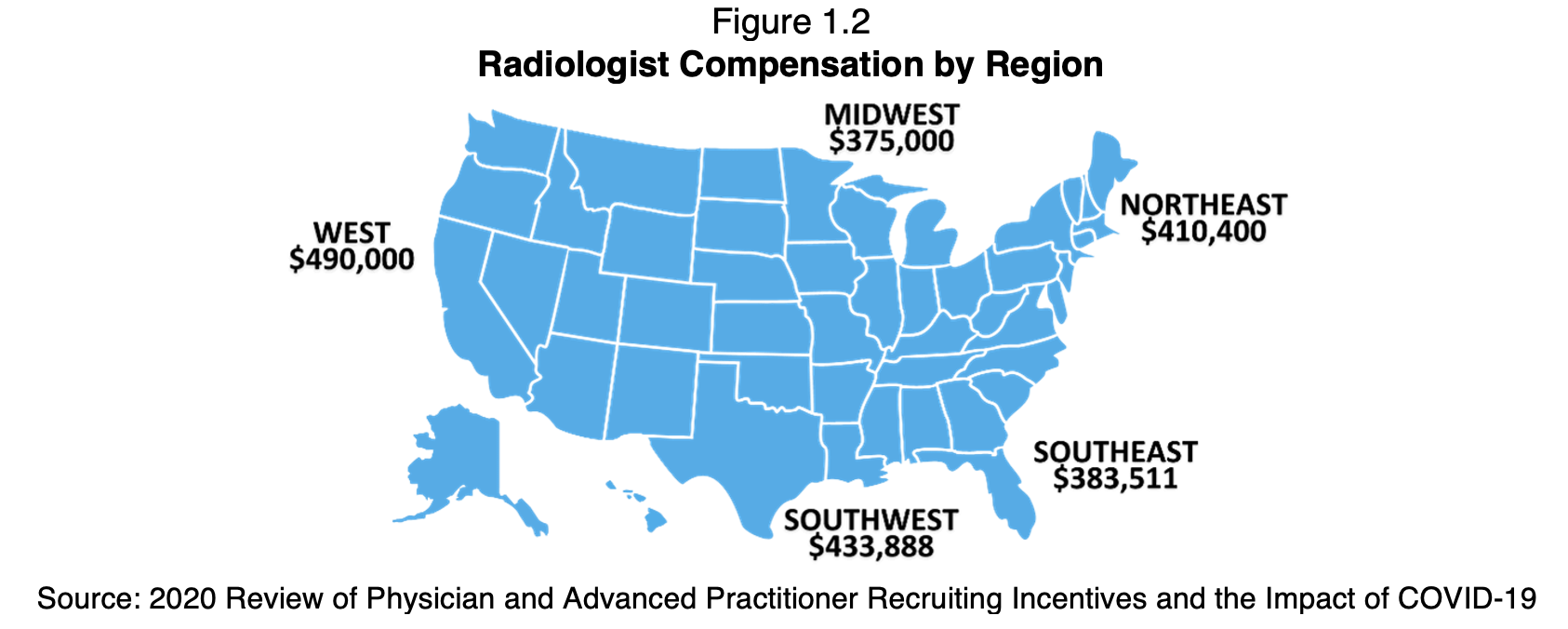
It’s also important for radiologists looking to change jobs to put higher compensation into context. Interestingly — although perhaps not surprisingly — we find higher average compensation in geographic regions (see figure 1.2) where the rise in the number of Medicare beneficiaries outpaces the number of radiologists. In other words, more money often means more work and more stress. This is most pronounced in the western U.S., which has both the highest salaries as well as the largest disconnect between new patients entering the Medicare system and new radiologists entering the field.
Beyond a paycheck: Radiologists are asking for more (or, in some cases, less)
While some job-seekers may be eager to seek out higher-paying positions no matter how difficult the working conditions may be, others are looking for something different: a better quality of life. During the pandemic, as the U.S. workforce shifted to accommodate more flexible working arrangements and more remote work, radiology was no exception. Radiologists, including those who usually work in the reading room of a hospital or imaging center, began reading from home. Many discovered that the work lends itself quite well to remote arrangements — perhaps even uniquely so in the medical field.
But while radiology groups were willing to experiment with remote work on a temporary basis, some are now calling their radiologists back into the office — or at least starting to message that they’ll be doing so soon. In general, these practices still aren’t optimally set up for remote reading. Some seem to be moving to hybrid models, but few seem to be ready to allow fully remote work.That doesn’t change the fact that not everyone is ready to go back to the office. On a weekly basis, I interview radiologists who have been called back but are finding it difficult to grapple with the idea of resuming their daily ritual of waking up early, putting on uncomfortable clothes, staying out at work all day, and coming home late. With the pandemic offering an opportunity for many radiologists to experience working from home for the first time, many discovered clear and perhaps unexpected benefits: more time with loved ones, a greater capacity to care for young children or elderly parents, and daily delights like the ability to take a break to eat dinner with their family every night, skip the daily commute and wear whatever they want. For those who adapted to this new-found freedom, the looming “return to normalcy” poses a threat to the mental balance they’ve enjoyed.
I’ve spoken to dozens of radiologists that, yes, care about getting a good salary, but also care about their quality of life. The pandemic has opened their eyes to a new way of living, and they don’t want to give that up. Among other things, they’re looking for flexible schedules with the ability to schedule their work around their personal life — whether that means holidays and weekends off, a one-week-on, two-weeks-off schedule for those reading nights, or seeking out jobs that don’t involve hours of commuting time each week.
For those physicians, teleradiology can be the holy grail, and I’m happy to say that many of them have joined us at vRad. They can set their own hours — typically with a seven-day-on, seven-day-off schedule — and work from their homes, while still getting very fairly compensated. They escape office politics, and they work at their own pace. There’s no pressure to finish out their list; at the end of their shift, any studies they haven’t looked at will be passed to another radiologist. When they’re off, they’re off.
In contrast to the common myth that teleradiology is only for older radiologists nearing retirement, we’ve found that younger radiologists are choosing vRad for a variety of reasons often related to the quality-of-life benefits we’ve talked about. Our most common demographic by age, representing 33% of our hires, is the 40-49 age range — what many would consider the “sandwich generation” caught between caring for young children and elderly parents. Following closely behind is the 50-59 age bracket, representing 26% of our new hires.
Radiologists looking for remote work will be increasingly likely to find it. More than one-quarter (28%) of 200 consecutive diagnostic radiologist job postings we reviewed on the ACR job board were advertised as “remote,” compared with 72% advertised as “onsite.”
Future trends: Looking ahead in Radiology
Radiologists should still realistically expect to see higher workloads over the years ahead. Images per exam are increasing as are the overall volume of studies. That may result in rising worklist pressure and longer hours — at least at traditional, onsite jobs. This could exacerbate already-high levels of burnout, estimated at a remarkably high 45% in Medscape’s 2019 National Physician Burnout, Depression, and Suicide report. In 2018 — before the rising volumes we’ve seen recently — there were already an estimated 26,457 imaging procedures per full-time equivalent (FTE) radiologist, according to consulting firm Frost & Sullivan, compared with just 14,900 imaging procedures per FTE radiologist a decade earlier in 2008.
In the meantime, there are some early indicators that we could be in the beginning stages of additional radiologists entering the field, which could help alleviate current job market pressures over time. First, we’ve seen an uptick in residency matches (see Figure 1.3); after a drop in fill percentages in 2020, both diagnostic and interventional radiology programs are trending higher.
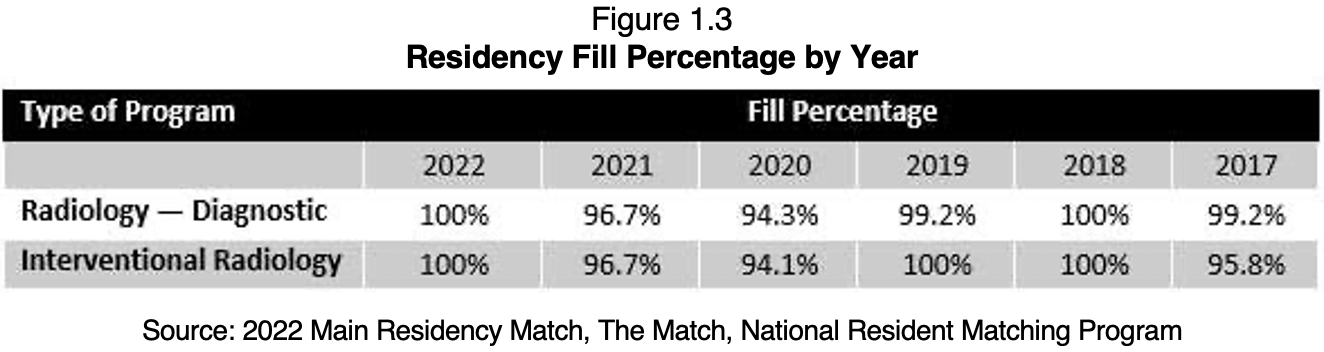
Additionally, in light of Congress passing the Consolidated Appropriations Act of 2021 — which allocates 1,000 new Medicare-funded physician residency slots — the ACR has taken the initiative to advocate for an increase in radiology residency slots. This could bode well for even higher numbers in the future.
As you’re evaluating your next career move, I hope you consider vRad. Practicing radiology from home can be very rewarding for radiologists of all backgrounds. If you’d like to speak to me directly, please request to be contacted here and mention my name. I’d be happy to share my experience and answer your questions.
