Artificial intelligence ROI considerations in radiology
Artificial Intelligence use has surged in radiology, promising increased efficiency, accuracy and patient outcomes. However, while AI might aid medical imagers and improve care, assessing the return on investment becomes a critical consideration since there is little to no reimbursement.
"One of the most important things to think about these days with AI, if you're going to get it deployed, is you need to have an ROI. AI costs money and if it's going to be sustainable, you need someone to pay for that," Nina Kottler, MD, associate chief medical officer for clinical AI at Radiology Partners, said in an interview with Radiology Business at the Radiological Society of North America 2023 meeting. "Payers aren't really paying for this. These days a lot of hospitals are losing money, so the ROI for them is if you can bring in more dollars into their system, or if you can decrease their costs."
Kottler also is an associate fellow of the Stanford Center for Artificial Intelligence in Medicine and Imaging, on the steering committee for RADEqual, and serves on several committees for RSNA, the American College of Radiology and the Society for Imaging Informatics in Medicine. She is a key figure in radiology AI and highlighted essential factors in understanding the ROI of AI adoption in radiology during a RSNA session.
While there are some reimbursement codes for a few new AI technologies, she explained ROI may not be monetary in the form of a direct reimbursement. Instead, ROI is often in the form or better efficency to enable radiologists to look at more studies of provide more information to referring physicians, or offering better patient outcomes by catching more disease and incidental findings. By helping to appropriately identify more patients with health issues, this can translate into more downstream services and therapies that a health system can bill for.
"You can bring in more dollars if you could get more imaging exams done, and from a procedure standpoint if you get more patient admissions," Kottler said. "Now of course we want these to be appropriate ones, but AI can help with those things. Decreasing cost is another way to do it. For instance, moving people through the emergency department more appropriately, more quickly, then you can decrease cost to a health system. Decreasing costs in admissions or if the length of stay is decreased, then you're getting the same dollars. But if the cost is decreased, those things can pay for the AI system."
Kottler emphasized that while physicians prioritize creating value for patients, deploying AI in healthcare demands sustainable financial models. Identifying stakeholders—hospitals, radiology practices, referring clinicians, payers (including Medicare and private insurers), and patients—can help delineate who bears the cost burden and who reaps the benefits. Direct patient payment for AI tools is not considered feasible, she said.
Challenges in AI reimbursement
Reimbursement remains a significant hurdle in AI adoption. Current payment structures, including intermittent reimbursements for certain Category III CPT codes and temporary payments like the Medicare Coverage of Innovative Technology, underscore the inconsistencies in funding AI initiatives.
The Centers for Medicare and Medicaid Services pays for some types of AI, if they are included in CMS programs. Often it is a temporary payment and only available for something that improves patient outcomes, often for technologies designated in the FDA Breakthrough Devices Program. Kottler said the CMS New Technology Add-on Payment offers payments for a three-year period to promote use of the technology. This option was used for some of the new stroke AI detection algorithms a few years ago, she noted.
More recently, CMS created the Transitional Coverage of Emerging Technologies, which offers temporary payments for AI technologies that earn an FDA breakthrough medical designation. "Medicare is only going to do a few of these per year, but it is a temporary four year coverage. But the vast majority are not getting paid for by payers," Kottler said.
Many AI vendors will say they have a CPT code from the American Medical Association, but these are usually Category III codes for tracking use of a new technology. However, the code provides data to the AMA to determine later on if providers are deploying the technology, and to help determine if it should gain reimbursement.
Hospital system ROI using AI
For hospitals operating on thin margins in a fee-for-service model, AI must demonstrate the potential to either increase revenue or reduce costs, Kottler said. AI needs to show the ability to streamline patient admissions, expedite emergency department processes, and decrease lengths of stay.
"For radiology, it's really about increasing efficiency so you are able to do more with the same amount or less effort...That means I could either finish my day earlier, or if you want to bring dollars in the system, you can do more and you can bring more exams in. And that's how you pay for those things," Kottler said.
Radiology practice ROI for quality and efficiency
Efficiency stands as the primary ROI metric for radiology practices. AI tools that enhance reporting processes, reduce the mental load on radiologists, and improve workflow efficiency hold immense value. Kottler emphasized the importance of utilizing AI tools to enable radiologists to do more with the same effort or less, thereby increasing productivity without compromising quality.
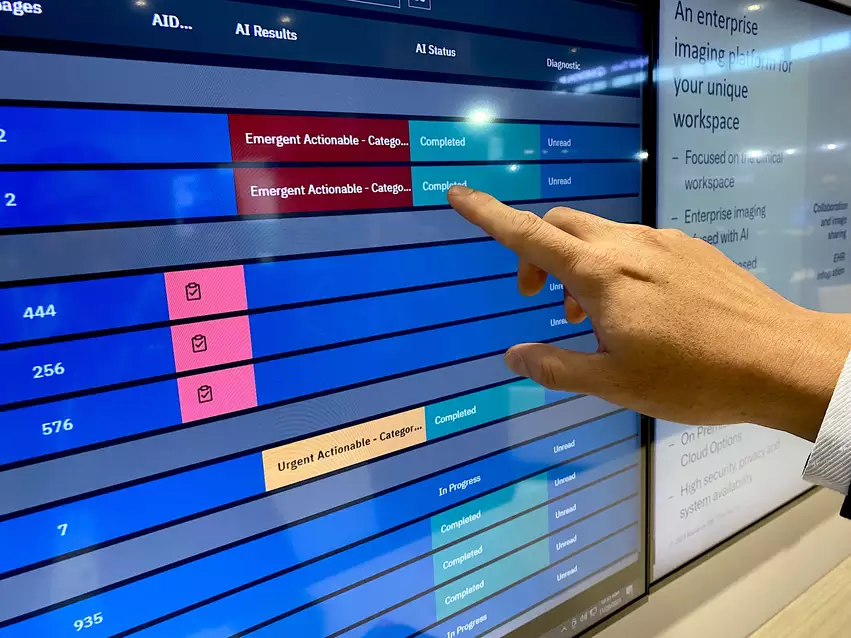
AI tools, particularly in computer vision-based applications like computer-aided detection, have shown promising results in enhancing radiologist accuracy. Such tools can increase detection rates for various pathologies, significantly benefiting patient outcomes. Additionally, AI aids in quality assurance by serving as a "second set of eyes" for radiologists and reducing mental fatigue, leading to better workday outcomes.
"Computer vision tools like CAD for triage are probably the most common kind of AI that we are seeing out there. There are tons of AI triage. These tools are not FDA cleared for detection, so what they do is they notify the radiologist about a certain finding being present. And then you can move that study up in the work list. What we found, both with that kind of AI tool and also with a detection tool, is that both of them can increase the radiologist's accuracy," Kottler said.
At her practice, AI tools helped increase detection up from 5% to 300%. The crazy number of 300% was for automated rib fracture detection in outpatient CT scans, which is often something the radiologist is not looking for specifically.
"In general, enhanced detection rates we are finding on average are 10%-20%. And those are actual true positives, real things that are there, whether it's breast cancer, pneumothorax, pulmonary embolus or intracranial hemorrhage. All of these findings are then translating into patients that are getting treatment. And so the hospital benefits because the patient then goes for procedures and get cared for, and that's also beneficial for the patient," Kottler said.
AI may help address the shortage of radiologists
There currently is a massive shortage in the number of radiologists to fill open positions. The shortage was known to be growing prior to COVID, but the pandemic greatly accelerated the problem with many radiologists becoming burned out or concerned about decreasing reimbursement and deciding to retire or leave clinical work as part of the Great Resignation. Medical schools are not graduating enough radiologists to fill vacancies and there are even fewer radiology residency slots available. This has many health systems considering what AI may be able to do to make the radiologists they do have more efficient.
"The AI that we are finding provides the most efficiency tends to be the ones that are working with the reporting tool, doing something with reporting. If you look at how much time a radiologist spends reading the study versus reporting, the vast majority is actually in the reporting, filling out the preamble of the report, information about the comparisons, the technique, etc., and writing or dictating the findings and impression. The other thing that we found in using some of those tools is they significantly help with the mental fatigue that a radiologist has at the end of the day. We are all burnt out because we're trying to do too much. And if you can decrease your mental load, decrease your mental fatigue, at the end of the day, it's a massive benefit," Kottler said.