Oncology imaging AI growing fast yet still in its infancy
If generalizable AI models are to meaningfully contribute to precision cancer care, they’ll need to incorporate not only imaging data but also digitalized clinical notes, biomarker assays and monitor readouts.
To be sure, effectively deploying these and other holistic data sources in real-world clinical settings is complex enough that developing the requisite technologies may take decades.
However, much will be learned along the way. In fact, AI in the service of oncology imaging will “change radiology in the coming years, leading to the optimization of imaging acquisition and discovery of clinically relevant biomarkers for cancer diagnosis, staging and treatment monitoring.”
The words are from neuroradiologist Melissa Chen, MD, of MD Anderson Cancer Center and fellow researchers who describe the promise and the problems in a paper published Sept. 29 in European Journal of Radiology Open [1].
One Day Deep Learning Will Help Solve Clinical Challenges at Bedside, Scale
Chen and co-authors expect AI to drive oncologic imaging across four overlapping yet discrete spheres of algorithm development. These are acquisition optimization, cancer screening, tumor response assessment and treatment planning.
Together, forthcoming findings and fine-tunings around AI-powered imaging in these areas will, the team suggests, “pave the road for future clinical translation in precision oncology.”
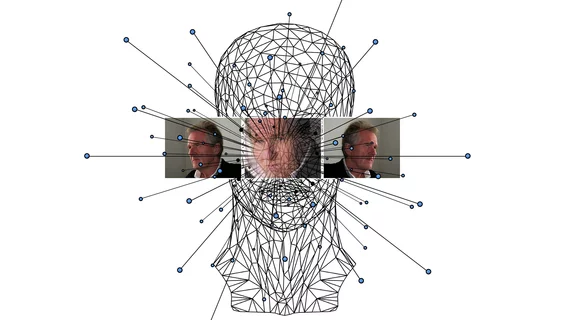
Where histopathological and molecular contributions can be biased by intratumor heterogeneity, Chen and co-authors note, imaging “offers a unique path to provide a holistic and dynamic view of disease at the whole organ or whole patient level, moving the assessment of cancer patients toward personalized oncology.”
Deep learning in particular stands to parse imaging patterns with heretofore unattainable sensitivity, the researchers suggest.
“Distinct from radiomics, which heavily relies on empirical knowledge, deep learning provides an end-to-end solution approach that can automatically learn by correlating raw data with ground truth,” they write, adding that deep learning systems will eventually prove sufficiently precise that they can help solve clinical challenges at the bedside and at scale.
So Many Software Packages, So Few Clinical Deployments
Tallying the FDA-approved AI applications related to oncologic imaging as listed by the ACR’s Data Science Institute, Chen and colleagues found more than 50 software packages in nine categories.
The top category is breast lesion characterization, with 12 applications, followed by image quality improvement and radiation treatment planning (10 each) and pulmonary nodule detection (nine).
The list is rounded out by prostate lesion characterization (six applications), PET image denoising (three) and brain tumor segmentation, lesion measurement comparison and liver lesion characterization (one each).
“Despite [this] growing body of evidence supporting the future utility of AI in oncologic imaging and a growing number of oncologic related FDA approved AI algorithms, clinical applications and adoption have been limited,” the authors report, citing earlier studies that back the point.
With that the team enumerates specific challenges standing between algorithm development and clinical adoption in AI-powered oncology imaging.
AI That Makes More Work for Radiologists ‘Will Not Be Adopted’
Among the hurdles they name are these five:
1. Access to a diverse and vast amount of data. This might be considered a good problem to have, but it “remains a critical bottleneck in the creation of robust and clinically useful models,” Chen and co-authors remark.
2. Privacy concerns and regulatory barriers are a major hindrance in the creation of such large datasets. Federated learning may offer relief, using local resources to train parts of a centralized model, but “many challenges remain in the curation of these multi-institutional datasets, such as standardized inclusion of patient demographics, cancer type, staging and molecular features, as well as standardized imaging acquisitions.”
3. The need for rigorous clinical validation linked to patient outcomes is critical, and integration with IT systems and radiology workflows remains a work in progress. This is so despite progress made by ACR and RSNA to organize demonstrations to “engage with relevant stakeholders and develop standards to facilitate” both external clinical validation and broad IT integration.
4. With ever-increasing imaging volumes and workforce shortages, AI that increases the work time in a radiologist’s day will not be adopted. Enough said?
5. Algorithm interpretability has far to go before transparency becomes the norm and black-box outputs the exception.
‘Narrow AI’ a Fine Start for Next-Gen Algorithms to Build On
Chen et al. conclude by underscoring that AI’s promise is to uncover connections and patterns in data that would be all but impossible to discern by humans, including radiologists.
“An integrated analysis across different platforms”—not only those hosting imaging datasets but also text-and readout-based datasets as well—“will further improve AI model performance” such that the technology can offer a “comprehensive and dynamic view of heterogeneous cancer,” the authors comment.
However, existing AI studies involving oncology imaging have mostly concentrated on answering specific clinical questions. They’ve used structured data for inputs and delivered simplified clinical outputs. This, the authors point out, is known as “narrow” AI.
More:
Given the complex nature of oncology, generalizable AI algorithms built on multimodal real-world data will become the next-generation approach to make real clinical impact. … [R]adiologists can and will play a leadership role by directing ongoing AI research efforts to address the most pressing clinical challenges rather than comparing AI systems versus human experts. These new algorithms will be welcomed and adopted to benefit cancer patient management.”
The paper is available in full for free.