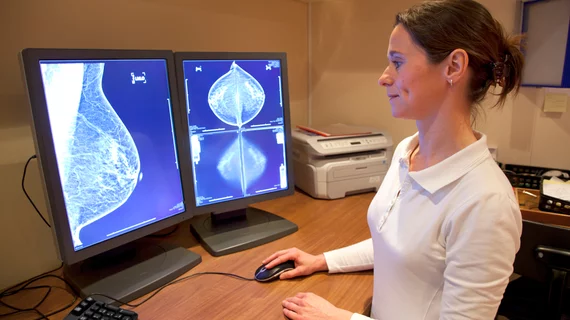
Second-opinion interpretations of breast imaging studies: Are they worth the additional resources?
Seeking second-opinion interpretations of breast imaging studies in patients not presently diagnosed with breast cancer can provide significant value, according to a new study published by the Journal of the American College of Radiology.
“At our institution, outside-facility images are uploaded into our PACS, and available outside-facility reports are routinely scanned into our electronic medical records system,” wrote Lauren Q. Chang Sen, MD, department of diagnostic radiology at the University of Texas MD Anderson Cancer Center in Houston, and colleagues. “A formal second-opinion interpretation is then rendered by a breast imaging specialist. The patient or the patient’s insurance company is billed for the second interpretation. This process can be time-consuming and incurs additional costs.”
The authors examined more than 2,000 second-opinion interpretations rendered at their own facility from Jan. 1, 2010, to June 30, 2014, of mammograms originally performed at outside facilities. Overall, the BI-RADS categories assigned at outside facilities and at the authors’ own facility were discordant more than 35 percent of the time.
More than 28 percent of patients originally assigned a BI-RADS category of 4 or 5 at outside facilities were assigned a BI-RADS category of 1, 2 or 3 by the second-opinion interpretation. In addition, more than 20 percent of patients originally assigned a BI-RADS category of 1, 2 or 3 at outside facilities were assigned a BI-RADS category of 4 or 5 by the second-opinion interpretation. This revealed 23 cancers, 15 high-risk lesions and 151 benign lesions. (One high-risk lesion was later upgraded to a cancer, meaning 24 cancers were revealed.) Eighteen of those cancers “reflected true additional breast cancer detection resulting from second-opinion interpretation.” The positive predictive value (PPV) for the number of cancers diagnosed among all recommended biopsies was 9.4 percent. The PPV for the number of cancers diagnosed among all biopsies recommended and performed was 9.5 percent.
“These results support the positive impact of second-opinion interpretation documented previously,” the authors wrote, citing numerous other studies that have reported a significant number of changes in the surgical management of breast imaging patients.
“In contrast to previously published studies, our study included only patients without a concurrent diagnosis of breast cancer, and a positive outcome of second-opinion interpretation was established,” the authors added. “The 18 additional breast cancer cases detected on second-opinion interpretation in our study translated into an 8 of 1,000 false-negative rate in our cohort (18 of 2,253).”
Chang Sen and colleagues also noted the impact second-opinion interpretations had on the health system and on patient anxiety.
“Although 11 patients for whom biopsy was not recommended on the basis of second-opinion interpretation ultimately underwent biopsies of the breast within two years, the overall outcome was 76 fewer patients undergoing biopsy, which reduced the cost to the health care system and patient anxiety related to the biopsies,” they wrote.