Radiology departments are well-positioned to champion the implementation of 3D printing services at the point of care, according to a new analysis published Friday in RadioGraphics.
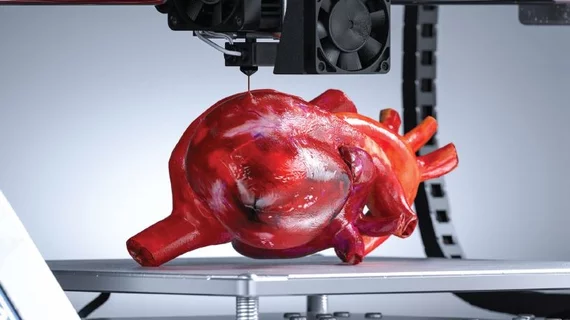
The use of such technology has grown in medicine but may remain a novelty to some radiologists. While not used for interpreting medical images, it can prove useful in planning complex surgeries or interventional radiology procedures, one editorialist noted.
Use of these models is rapidly expanding, allowing providers to produce patient-specific, highly customized models of the anatomy. Experts believe the specialty can play a central role in spreading this technology in their own organizations.
“As the use of 3D printing becomes even more widespread, and as evidence accumulates in the literature, radiologists are centrally positioned to add value to the multidisciplinary care of patients and to assist our surgical and medical colleagues in ways beyond image interpretation,” radiologist Sarah Bastawrous, DO, an associate professor with the University of Washington School of Medicine in Seattle, and co-authors from several institutions wrote Feb. 4. “Incorporating the potential and strengths of 3D printing technology into radiology departments can allow radiologists to take the lead in this emerging field and enhance our contributions to healthcare.”
Bastawrous et al. offer a practical guide for launching a 3D printing service, with gaining leadership support one critical step. Decision makers may request a formal business plan, detailing start-up and maintenance costs along with return on investment. In the writers’ experience, 3D printing ROI typically comes in four forms: cost savings and avoidance, access to care, innovations in treatment, and patient outcomes. As far as the latter, the writers gave the examples of decreased radiation dose stemming from reduced fluoroscopic exam time, lower dosage of IV contrast materials during certain interventional procedures and improved surgical performance.
While 3D printing technology has become more affordable, startup costs can be “substantial,” the authors noted. The initial investment may tally between $10,000 to $30,000 for a small printer, starting materials, software, borrowed personnel time and space. But it can soar to “several hundreds of thousands of dollars” for a full-time lab with dedicated employees, FDA-approved software, and high-end printers. Licensing fees, post-processing software and specialized staffers can add even more to the budget.
There are also complex reimbursement and regulatory considerations. Those considering launching such a service in their radiology department should consider the primary mission statement of the endeavor, given possible payment challenges, David Ballard, MD, wrote in a corresponding editorial.
“Can radiology departments run such a laboratory as primarily a clinical service and expect it to be a profitable investment? With current limited reimbursement options, the answer is likely no, without hospital, institutional, or donor support,” wrote Ballard, with Washington University’s Mallinckrodt Institute of Radiology in St. Louis. “Hospital support and reimbursement agreements can be pursued to potentially break even and at least cover operational expenses of a 3D printing laboratory,” he added later.
Read much more in the Radiological Society of North America’s RadioGraphics journal here.