How radiology should prepare for AUC clinical decision support reporting requirements
In an effort to reduce the number of inappropriate advanced imaging exams, the Centers for for Medicare and Medicaid Services (CMS) plans to implement a new requirement for appropriate use criteria clinical decision support (AUC/CDS) software consultation documented on all radiology requests. These CDS systems are supposed to be in place and in use beginning Jan. 1, 2023.
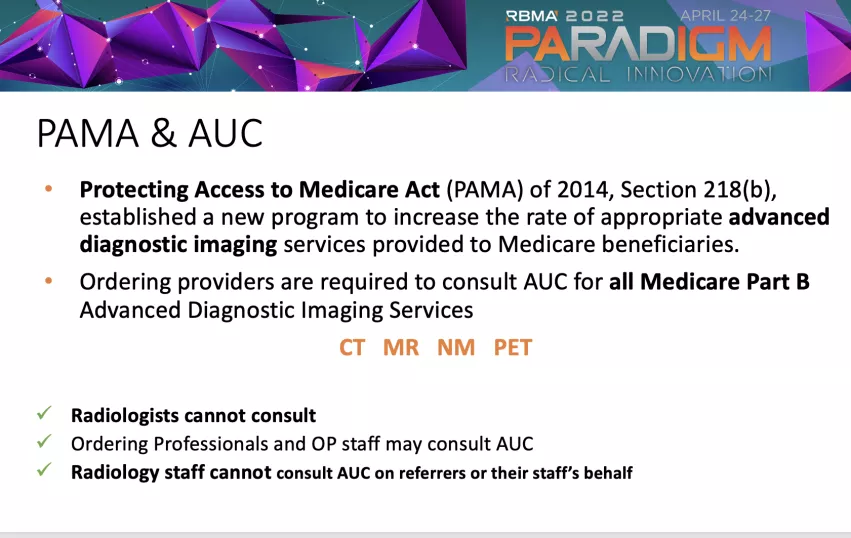
CMS said after Jan. 1, 2023, claims submitted without compliance certificates from CDS will be rejected. This is a mandate written into the Protecting Access to Medicare Act of 2014 (PAMA)
The AUC/CDS mandate was a big topic of discussion at the Radiology Business Management Association (RBMA) 2022 meeting in late April. RBMA offered a session to provide a refresher on the AUC/CDS requirements and discussed methods to be prepared.
Lisa Mead PSO executive director, Strategic Radiology, spoke at the session. She reviewed the components of the AUC/CDS program mandated by PAMA, and the methods that can be utilized by practices to successfully coordinate hospitals and referring providers in program implementation. She addressed questions regarding the CDS mandate.
Multiple delaying in implementing appropriate use clinical decision support
This requirement was originally supposed to go into effect in 2017, but its implementation has been delayed several times. Several medical imaging societies are calling on Congress to repeal the AUC/CDS mandate because they believe it will cause delays in care, involve more administrative staff time and add costs to healthcare. There are also concerns that delays in updating CDS software with new guidelines and expert consensus recommendations will cause billing issues and additional staff time to address.
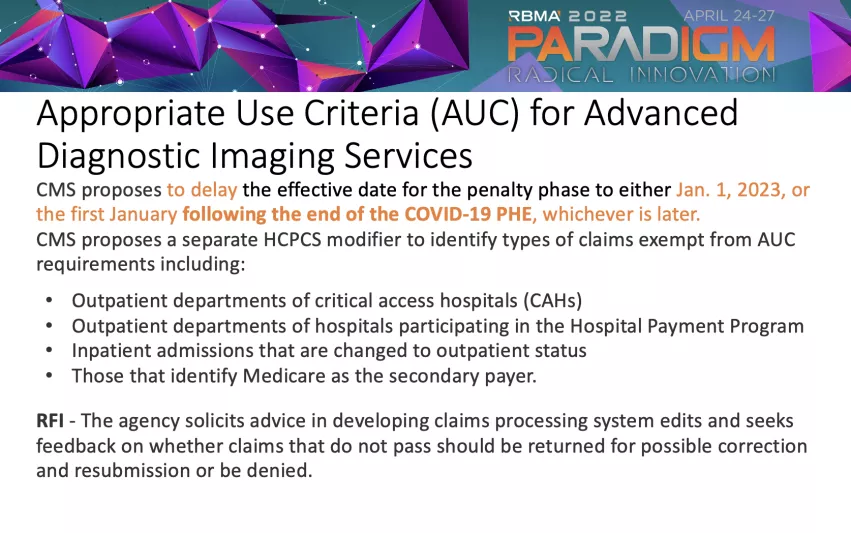
"We have been delayed in the penalty phase for four times," Mead explained. "We will see if it will be delayed again when the final rule and the preliminary rule for the physician fee schedule comes out later this year. They have given some wiggle room right now. If there is a delay it will be for the penalty phase, which will start in January of 2023, or the first January after the end of the COVID public health emergency."
Referring physicians must use CDS software to document AUC for the imaging exams they order
Mead said under the rule, the furnishing provider for the medical imaging — the radiology group or the hospital providing the radiology exam and the read — will have their claim adjusted in the penalty phase.
"But, it is the ordering physician or provider that is required to consult the clinical decision support mechanism and provide a code modifier to the furnishing provider to put on the claim," Mead said. "The radiologists and radiology staff cannot consult AUC on their refers' behalf."
She explained this clinical decision support mechanism needs to be a part of the image order portal. This can be built into Epic, Cerner, NextGen or whatever their electronic medical record (EMR) system is. If CDS is not built in to the order portal, the radiology provider needs to furnishing referring providers access to a clinical decision support mechanism they can use during the ordering process. She said the CDS software is relatively easy to use so most referring physicians should not have an issue with it.
"So they'll plug in what they're looking to order and possibly the symptom ICD-10 code, and then the system will rank the exams, or provide what is the appropriate exam. They can bypass it and still order it. They will have a code that says that they're not in agreement with the CDS advice," Mead said.
Radiology needs to educate referring physicians that AUC CDS is important
Because the referring physicians are the ones required to consult CDS software to document the orders they are entering, Mead said it is on radiology practices to explain why this is really important. Mead said they need to explain why this is needed and how to use CDS, because otherwise it may cause reimbursement issues.
"I think we're still at the large percent of referring physicians aren't really aware that this is going to impact them," Mead said. "You should you be talking to referring providers, whether that's your hospital, regional radiology providers, cardiology or orthopedics, anyone that's using advanced imaging. It's a little bit difficult because you're asking people to do something that they don't see a stick at all. We as radiology furnishing providers are in the penalty end of things. So it's up to us to educate and make sure they understand what it's going to look like."
She said the CDS systems themselves are readily available. These systems are built and then certified by CMS. Part of the PAMA rule is that radiology practices or the hospitals have to make the CDS software available in a free portal, or make the tool available on their websites if it is not already built into their ordering portals.
"I have been telling radiology practices to educate and provide information to the referring physicians, because it really starts with them," Mead said. This includes discussion about why this new rule is going into effect, its impact on billing, what the plans are to make CDS available and how to use it.
Implementing clinical decision support tools for imaging
Mead said radiology practices, hospitals and outpatient imaging centers definitely should be talking to their risk provider and finding out what tools are available through their online portals for CDS on orders. There are a couple qualified decision support mechanisms they easily can implement through their portal for their referring physicians to access, she said.
If there is already CDS software built into the system they use to order imaging exams, that is always the best way to go.
"You're already using this in your office. Now it's just clicking on another tab. I think it's important that they contact their provider, contact their hospitals, especially if they're critical access hospital," Mead said.
She noted that CMS has different rules for critical access hospitals related to the CDS mandate, making them exempt. But, she warned there is a lot still up in the air on how that billing works if you are the physician provider in that relationship.
CMS CDS rule is designed to improve quality of care and reduce costs
Mead said the main goal of the AUC CDS requirement is to improve the quality of care given to patients by making sure they get the right test for the clinical question being asked. This also can help reduce overall healthcare costs by reducing the number of expensive imaging tests that are ordered.
"Radiologists and the American College of Radiology (ACR) put together the decision support tools," Mead said. "It is designed to decrease over utilization, make sure that we're doing the right exam at the right time. The burden of the penalty is not so great for the radiology furnishing provider, but it is really designed to help educate referring physicians."
Tracking who is not using CDS on imaging exam orders
"I'm telling the everyone to keep track of who is not providing the code so that you can go back to the referring physician, or team up with your hospitals, and educate them," Mead explained. "I think there are lots of ways to go about this without having to deny care. Radiologists I think they do a good job of trying to educate providers through protocols, calling people back and telling them this isn't the right exam. They can say, 'I see you've done this, you know, I think we should do this.'"
Expect trial and error and revisions to the CMS CDS requirements
Like other Medicare programs implemented in the past, the government will start off with what seems like the best course of action and then look at how things are going, gather feedback from providers and make changes over time.
"I think we're supposed to be approaching it as a learning opportunity right now," Mead said.
Like the hospital metrics from 20 years ago, she said things start off as voluntary, but will become mandatory with incentive payments to follow the rule, or penalties in payments if the new rule is not followed. "I would imagine that there is going to be a stick at the end of the whole thing," Mead said.
Watch the VIDEO: Preparing for radiology appropriate use criteria clinical decision support reporting requirements — with Lisa Mead, Strategic Radiology
Related RBMA and Appropriate Use CDS Mandate Content:
VIDEO: Imaging societies ask Congress to repeal appropriate use decision support mandate
VIDEO: The importance of the Physician Practice Information Survey and its impact on radiology reimbursements — Interview with Linda Wilgus, CPA, CMPE