Is Medicare’s appropriate-use criteria program doomed? ACR chief discusses what went wrong and how it can get back on track
Advocates of radiology’s march toward value were dealt a blow back in July when the federal government announced it was pausing the appropriate use criteria program. Can AUC get back on track or will it languish?
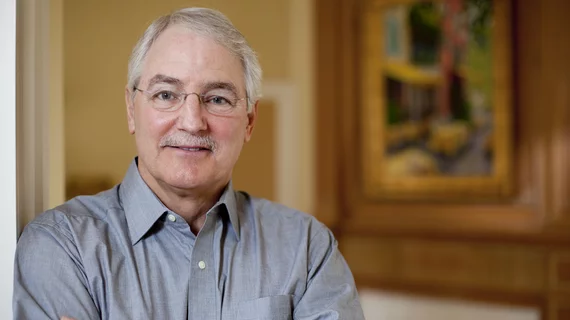
As next month marks 10 years since Congress passed the Protecting Access to Medicare Act, which set up the mandating of AUC, Radiology Business sat down to discuss the program with outgoing American College of Radiology CEO William Thorwarth Jr., MD, who is retiring this summer.
Here are excerpts, lightly edited for clarity and conciseness.
Radiology Business: What was your reaction when you heard about the AUC pause? Was it disappointment or were you expecting this?
William Thorwarth: Certainly, disappointment because we do think this kind of use of physician-developed, evidence-based, transparent criteria is a huge step up from the prior authorization that has been the bane of existence for referring providers—and not just in radiology. I'm talking about in pharmacy and other areas of healthcare as well. We believe [AUC established] a better process, and so we were disappointed. But because of the challenges we'd seen for years, we were not totally surprised. That's why we started the conversations with CMS several years ago.
Where does this rank on your list of setbacks or disappointments over the past 10 years with ACR? Does this make the list?
Oh yeah, I think so. We've put a tremendous amount of commitment and effort into this, both volunteers and staff, because we think it really is a better process, a much more educational, long-term process. ACR is committed to [AUC] and has been for going on 30 years now. Implementing it in healthcare would have several positives. For starters, patients would only get tests that will be appropriate and necessary. The criteria will say if there's no reason to do an imaging test. And from the provider's perspective, I'm sure you've read all the literature about physicians being frustrated, feeling the prior authorization process interferes with their ability to take care of their patients. We think that they'll likewise benefit from this [AUC] and, with the consultation of the appropriateness criteria, learn what's the best test, given clinical circumstances.
From a financial standpoint, there's no question that this [AUC] shows an improvement in care and appropriateness—and also significant savings. So, the taxpayer benefits, potentially, or at least the Medicare fund would benefit, from implementation of this as well. That's something we're really committed to, and we want to get [AUC] across the finish line because, quite frankly, the infrastructure is there and the work has been done. We continue to upgrade. We have a number of panels that upgrade these hundreds of clinical indications, over a thousand different variants. We've got the material ready to go and just want to see it implemented. It's better care.
Why is it taking so long? It was way back in 2014 when Congress passed PAMA.
The very prescriptive language of the original law required a real-time, contemporaneous component. Just to paint the picture, a physician is seeing a patient in their office. They want to get an MRI of the lumbar spine, and again, this is only for advanced diagnostic imaging, so CT, MRI, nuclear medicine and PET. But they have a patient in their office, and they think that an MRI of the shoulder or lumbar spine is an appropriate test to get. They consult the criteria, and either the patient has clinical symptoms that warrant the imaging, or they're guided to get a different test or no test at all.
But by the original PAMA law, [checking the criteria] had to be done at that time [of ordering the imaging]. If the physician then sends the patient to, say, a radiology facility and they haven't got an AUC scoring number that says, yes, this has been cleared by Medicare and the appropriate consultation of criteria has been performed, then the facility is on the hook. If they perform the test without that documentation, they won't get paid, according to the original legislation. So, the real challenge was that particular requirement of real-time contemporaneous documentation of the consultation of the criteria.
Could you tell us a little more about the legislative fix and Congress's receptiveness to it?
Our conversations with staff members, committees of jurisdiction and members of Congress is that, yes, they'd like to see this [AUC] get across the finish line. They passed it with the intent that it be implemented. They understand the challenges that have been faced by CMS. So, we're hopeful that we can find a legislative vehicle this year to attach the modifications that would need to take place.
We are likewise assured in our conversations with CMS that, given those changes, they would be able to proceed. That was evident in the final rule. They say they find AUC very valuable; they recommend that its use continues. And, again, in their words, CMS estimated somewhere around $700 million a year in potential savings, just for imaging. If we are willing to be the prototype—if this works—you can imagine they could expand it to other diagnostic testing, durable medical equipment, pharmacy, etc., so that the best care can be delivered, and the referring providers get informed of the recommendations in a prospective manner.
Why is it so hard to get anything involving medicine through Congress nowadays?
It's largely related to costs, and we are hoping that our proposal can get through the Congressional Budget Office, given that large savings figure. We had some independent consulting work done by the Moran Company that also put it at somewhere around $2 billion over 10 years. But to answer your question about the challenges of getting through Congress right now, so much of it has to do with the costs. We would hope to get a [CBO] score that would show us to potentially be somewhat of a pay-for for some of the other things that are being considered, whether you talk about the Medicare fix or the Medicare Economic Index correction of the physician fee schedule and things like that. It really is the cost that holds up all of these things in Congress.
You mentioned the $700 million figure, referring to reduced spending on imaging. Could you talk about the challenge of convincing colleagues that this aspect of AUC is good for radiologists, even though it may be taking money out of their pockets?
I'd give two major reasons they should support this. One, everybody's in a workforce shortage. I just got back from the ACR-RBMA Practice Leadership Forum. Every practice there is trying to recruit. If you look at our career center over the past year, there have been 14,000 listings, with only 1,100 residents coming out per year. So, everybody is working full-tilt, and if we could eliminate some of the inappropriate exams, radiologists could concentrate on the exams that really are appropriate and need to be done. I do think that there's some real potential benefit from the standpoint of physician burnout.
Likewise on the referring provider side. If referrers could get guidance to the right test, then they don't have to read a report that says, ‘Well, this test was negative, but you really should have done this other test.’
We have to understand that Medicare is under a Congressional budget neutrality requirement. You can keep pushing volume, but then what happens is per-exam reimbursement is going to get ratcheted down, just as we see is happening in 2024. The correction of the conversion factor goes downward because it's working with a fixed pie.
I don’t think that the volume argument carries you very far when you realize that you're negatively impacting your per-exam reimbursement. For those who may want to hold onto volume, I don't see in my lifetime a place where radiology volume is going to drop off and people aren't going to have plenty of work to do.
CTA is one we have heard a lot about lately, where radiologists seem frustrated with the rising volume, and we’ve seen some research that says not all orders are worthwhile.
This is exactly the justification for the appropriateness criteria. If someone goes into an ER and they're a little confused, but they have no focal neurologic findings to suggest a stroke—or any evident need to subject them to a head CT followed by a CT angiography of the head and neck, with very low resulting yield—that's the kind of thing we'd like to avoid. There's good evidence out there to guide people to when a test is appropriate and when it really isn’t going to yield any benefit to the patient. In those cases, an imaging exam is just going to introduce unnecessary radiation and contrast exposure.
You talk about AUC being a preferred approach to prior authorization or radiology benefit managers. But those continue to be a thorn in the side for ordering providers and radiologists. What do you say to those who are feeling the weight of administrative burden and saying, ‘AUC is great, but I don't want another item on my plate’?
You have to start with the fundamental assumption that utilization management is going to occur. There's never going to be a time in medicine again in which everybody just does whatever they want. Given that, we think this is a far better avenue to get to utilization management.
Several states have developed, I don't want to call it gold carding, but facilities that have agreed to implement appropriate-use criteria have been afforded the option of not going through prior authorization. Both referring practices and radiology practices often are paying full-time equivalents to sit on the phone to try to work their way through a complex chain to get a prior authorization. In the meantime, legitimate patient care is delayed or sometimes not even being performed.
We think the combination of giving good guidance on the front end—having the educational benefit to the provider so they know next time I should or should not proceed with this kind of order, and then the benefit to the patient of not getting tests they don't need, but getting the appropriate tests at the right time, along with the savings to Medicare—it's a win-win-win, as far as we're concerned.
Hopefully we'll be able to convince the providers who may be reluctant to say, ‘yep, I know I'm going to need to do something. This is much better than the other costs, inconveniences and patient impact that goes on with prior authorization.’
And, if this [AUC] works the way you want it to, maybe payers will cool off a little bit on PA front?
Sure. It’s to their benefit as well. Payers have got the same staffing costs related to the prior authorization process. I don't know how many phone banks at the various insurers are doing this. Also, if you've got physician organizations like the ACR willing to participate in a multispecialty way of developing these new practice patterns, then they are not having to try and develop them themselves. There's a real benefit to the insurers to get on board with this [AUC], and hopefully they will see that.
I just want to ask you personally, why are you doing this? Why are you doing interviews about AUC when retirement is on the horizon? Why not just sort of sail into the sunset and not worry about this stuff?
I've been with the organization in a volunteer fashion or subsequently on staff for going on 40 years. We knew we had a complex spectrum of tests that were hard enough sometimes for radiologists to keep up with, let alone referring providers. I think we really did the right thing for the right reasons. We then realized, to take it to scale and have it be available at the point of care, we participated in the development of clinical decision support software that's available out there.
So personally, yeah, I'm committed to this in a big way. I'm becoming a consumer of healthcare in my age bracket, and, if one of my physicians decides they'd like to order such and such a test, I'd like them to get guidance as to which is the best, if any test is necessary at all.
Is it hard to go into retirement seeing AUC at the state it's in, where it is paused and not humming along up and running the way you wanted it?
Would we have preferred that it had been easy to implement and widespread and branching out into other modalities or other areas of medicine by now? Yes, we would love to see that happen. We respect CMS’s efforts.
You asked why this is taking so long. CMS did make progress on developing the qualified provider-led entity criteria to make sure that somebody can't just make up a list and toss that in. They did the qualified clinical decision support mechanism criteria. There was progress being made at each step along the way. It's just when we got to that final pull-the-trigger, let's get this implemented moment, we came across this challenge with that contemporaneous requirement. That's why we think that all the rest of the elements will stay in place. It just needs to be attested to and documented in a different fashion.
We really do hope that people don't get antsy, frankly, and start to think this is never going to happen. I do believe, with the congressional modification, it will move forward. This is going to become the standard of guidance for clinical care, not just in radiology, but across the board in the future.
Are you fighting anyone behind the scenes on this? I mean, is there someone lobbying against this that's leading to these delays?
To your comment earlier, there have been some specialty societies that have kind of resisted this and said, ‘Don't kill me with one more click.’ But again, we know utilization management is going to occur and so let's do it in the best physician-developed, guided, transparent fashion. There have been a lot of complaints that prior authorization can be kind of a black box where you don't know what's going on inside of it. I think we've got the backing of many who supported AUC in 2014 when the legislation went through, and now I think we can show them that this will not be a burden to the physicians, but rather something that saves them time and effort and money as well.
For more on what comes next with the AUC program, you can read this recently released backgrounder from the ACR, which led to this interview.