Opportunistic screening for fatty liver disease on CT and ultrasound is feasible, experts say
Opportunistic screening for fatty liver disease on CT and ultrasound imaging is a feasible strategy, experts advised Monday in the Journal of the American College of Radiology.
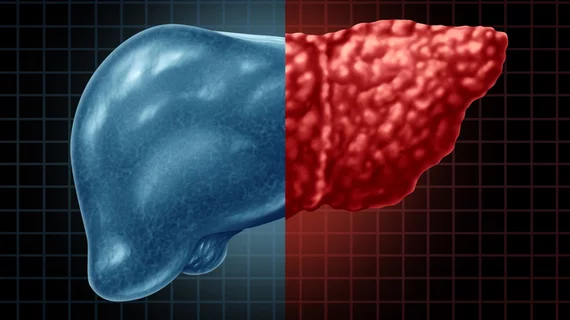
Hepatic steatosis is a common incidental finding on abdominal exams. However, physicians do not always denote it, despite its association with liver disease, cirrhosis and diabetes. Nonalcoholic fatty liver disease is a “significant” issue in the U.S., affecting a quarter of the population, with annual direct costs of $103 billion, Seattle researchers noted.
Wanting to bring greater attention to this issue, Virginia Mason Medical Center scientists inserted standardized text into rad reports of patients with incidentally detected liver disease. The change produced progress, with the inclusion of recommendations in reports leading to documented clinical follow-up in 52% of patients.
“Opportunistic screening for hepatic steatosis on routine abdominal ultrasound and CT is feasible and may help identify patients with increased risk for morbidity and mortality associated with [nonalcoholic fatty liver disease] and [nonalcoholic steatohepatitis],” corresponding author David Coy, MD, PhD, with Virginia Mason’s Department of Radiology, and co-authors wrote May 24.
To reach their conclusions, Coy and colleagues conducted a retrospective, single-center study at an urban teaching hospital. Starting in April 2016, rads began tagging abdominal imaging patients with hepatic steatosis discovered incidentally on CT and ultrasound. For those who met certain diagnostic criteria for this concern, rads inserted a voice note within the “impression” section of the report.
All together, they tagged 1,256 patients between 2016-2017, and physicians also reviewed their electronic medical records up through December 2018 to pinpoint any subsequent clinical action after the tag. Coy and co-authors discovered that a response was more likely among patients whose primary care provider ordered the CT or ultrasound scan. Same for those with exam results that were not urgent and who were in the ultrasound group.
Among 62% (or 777) of patients in the study, referring providers acknowledged the presence of hepatic steatosis in some fashion in the electronic medical record. In patients who received a clinical diagnosis, 70% had nonalcoholic fatty liver disease, 17% had alcoholic hepatitis, and 6% had nonalcoholic steatohepatitis (liver inflammation and damage caused by fat buildup).
“Though our results are favorable, future research may be needed to determine both cost and cost-effectiveness of opportunistic screening, as well as its effect on advanced patient outcomes such as development of cirrhosis, and associated comorbidities including diabetes and cardiovascular disease,” the authors cautioned.