VA telestroke program prevents unnecessary hospital transfers and improves rural outcomes
A new study of the U.S. Department of Veterans Affairs Veterans Health Administration (VHA) National Telestroke Program by the Regenstrief Institute and Indiana University School of Medicine shows the program prevents unnecessary hospital transfers for stroke patients. The program decreased the need to transfer patients to other hospitals by 60% after implementation.
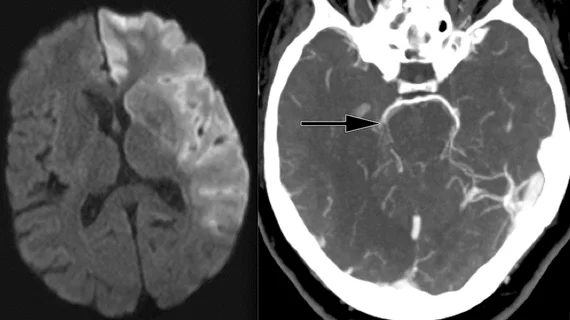
The program has made expert stroke care quickly available to patients, even at rural facilities with limited staffing. The telemedicine program connects a neurologist to the smaller clinic or a VA hospital where they do not have a neurologist staffed. A video assessment can be made of the patient and computed tomography (CT) medical imaging can be shared remotely to determine the type of stroke. This can help quickly determine treatment with tissue plasminogen activator (tPA), or transferring a patient quickly to a center that offers catheter-based thrombectomy to revascularize the patient.
The new study from the VA, Regenstrief Institute and Indiana University School of Medicine shows the telestroke program prevents unnecessary hospital transfers for stroke patients. The study was published online ahead of print in Neurology.[1]
“This analysis suggests that telestroke provides additional benefits for both patients and health systems,” said senior author Linda Williams, MD, a VA researcher and a Regenstrief research scientist in Indianapolis, in a press release about the study. “It increases care efficiency and cost-effectiveness, while further optimizing care for the patient who does not have to endure an unnecessary or even counterproductive transfer to another facility.”
How the VA Telestroke Program works
The VHA National Telestroke Program provides acute stroke care at facilities that do not have a neurologist available. Through a mobile device, a neurologist from the central hub is able to evaluate the patients and provide a treatment plan for the on-site staff to carry out. Some patients can be treated at the community facility, while others need to be moved to a hospital with a higher level of care, such as a comprehensive stroke care center. The neurologist from the central hub helps the on-site clinical team make that decision.
For this study, the researchers analyzed the number of patient transfers at 21 VHA facilities before and after the implementation of the telestroke program. They found the likelihood of being transferred to another facility decreased by 60% after the program’s implementation. The program also increased the chance that the patient received timely acute stroke treatment with thrombectomy.
“The VHA telestroke program facilitates timely assessment of stroke and elevates the level of care at smaller facilities, eliminating the need for many transfers,” Williams said. “This demonstrates another strategy to leverage telehealth in acute care settings while also reducing rural healthcare disparities.”
VA Telestroke Program increases care and improves outcomes for rural clinics
The VA National TeleStroke Program was launched early in 2018 and started with eight participating facilities. In the first six months of operation, 94 acute telestroke consultations were completed. Of these, 46% were diagnosed with stroke and 11% with transient ischemic attack (TIA). More than half of the veterans (56%) receiving a telestroke consultation were living in rural areas, and 2% were living in highly rural areas (defined by VA as “remotest occupied land areas”). There are 5.1 million veterans living in rural and highly rural settings, with 2.7 million enrolled in VA healthcare, according the VA's telestroke program website.
The VA created a hub-and-spoke model for VA stroke neurologists to cover 40 VA facilities through the telestroke program. The VA had plans in 2020 to expand to add 20 more to the program each year.
A recent study from March 2022 in Value in Health showed the VA Telestroke Program was associated with significantly higher rates of patients receiving guideline concordant care.[2] Compared with control patients, those treated in the telemedicine program were 14.3% more likely to receive tPA and 4.3% more likely to receive a thrombectomy (all P < .0001).
The study found the telestroke program was associated with $4,821 increased costs for patients with stroke in the first 30 days after the program. The authors said there were no observed savings over 12 months, and the added costs of care were attributable to higher rates of guideline concordant care.
Related Stroke Imaging Content:
Automated CT scoring system accurately predicts prognosis in stroke patients
New CT protocol uses scout images to expedite stroke patients' path to MRI
What decades of data tell us about stroke rates in the U.S.
Most Americans live within an hour of a stroke center
FDA warns providers about potential misuse of imaging-based software for stroke triage
Radiologists must change their approach to stroke care in the AI era
MRI findings associated with poor thrombectomy outcomes after stroke
Risk of recurrent stroke 48% higher among young marijuana users
References: