7T MRI scans provide a high-res look at how migraines affect the brain
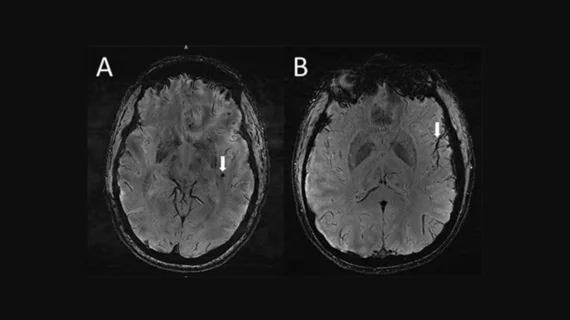
Using ultra-high-resolution MRI, researchers examining brain tissue in both chronic and episodic migraine sufferers have identified a significant finding: Compared with a control population, people with migraines have enlarged perivascular spaces in the central semiovale, the brain’s central area of white matter.
The study's authors will be sharing their findings at RSNA 2022 in Chicago, the annual meeting of the Radiological Society of North America (RSNA).
“Perivascular spaces are part of a fluid clearance system in the brain,” study co-author Wilson Xu, an MD candidate at Keck School of Medicine of the University of Southern California in Los Angeles, said in a statement. “Studying how they contribute to migraine could help us better understand the complexities of how migraines occur.”
Typically, the researchers noted, the fluid-filled spaces are affected by abnormalities at the blood-brain barrier and by inflammation. When they’re enlarged, it can be a sign of underlying small vessel disease.
In the instances of migraine patients, the researchers hypothesized that the enlarged perivascular spaces represent a disruption in the glymphatic system, which is responsible for clearing waste by eliminating soluble proteins and metabolites from the central nervous system.
However, there are still many unknowns surrounding whether the observed changes are a result of migraines, or a contributing cause.
Another key finding from the MRI study was a correlation between the quantity of the enlarged perivascular spaces and deep white matter hyperintensity severity.
“Although we didn’t find any significant changes in the severity of white matter lesions in patients with and without migraine, these white matter lesions were significantly linked to the presence of enlarged perivascular spaces," Xu said. "This suggests that changes in perivascular spaces could lead to future development of more white matter legions."
The study is the first to use 7T MRI to study microvascular changes in the brain due to migraine. There were just 25 participants analyzed: 10 with chronic migraine, 10 with episodic migraine without aura, and five control patients. The authors noted that the small sample size leads to an opportunity for larger studies in the future to learn more.
“The results of our study could inspire future, larger-scale studies to continue investigating how changes in the brain’s microscopic vessels and blood supply contribute to different migraine types,” Xu said. “Eventually, this could help us develop new, personalized ways to diagnose and treat migraine.”
Additional coverage of RSNA 2022 is available here and here.