NASA's Artemis 1 moon mission using phantom technology familiar to imaging specialists
While NASA's Artemis 1 space capsule is swinging around the moon in deep space during the Radiological Society of North American (RSNA) 2022 meeting this week, one of the most interesting medical physics experiments is underway 260,000 miles from earth. It is being done with the help of an RSNA attendee and incoming president-elect of the American Association of Physicists in Medicine (AAPM).
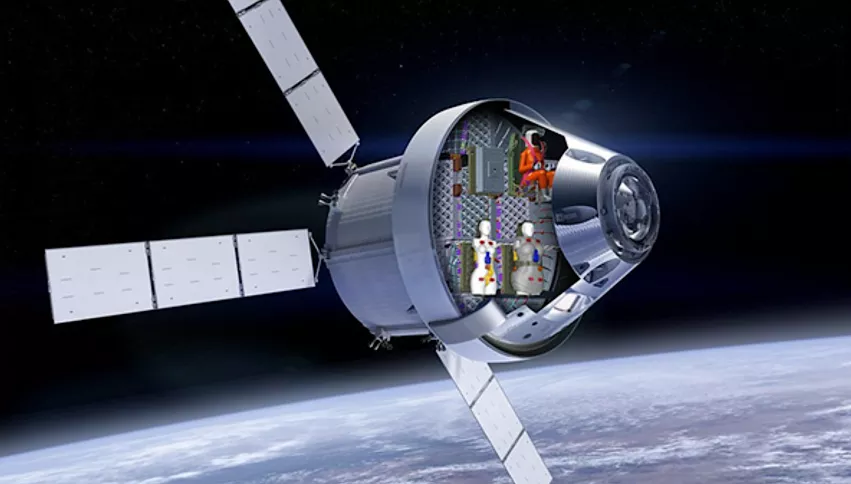
Duke University’s Center for Virtual Imaging Trials (CVIT) Director Ehsan Samei, PhD, the Duke University Reed and Martha Rice Distinguished Professor of radiology, medical physics, biomedical engineering, physics and electrical and computer engineering, is part of the team that developed the two specialized, medical-grade mannequin humans. The complex models are known in the medical world as phantoms, and they make up the simulated crew of this first Artemis mission. Samei took time during RSNA this week for an interview with Radiology Business.
Duke University bioengineers have been making virtual humans for the past 19 years for medical imaging research. With support from the National Institute of Biomedical Imaging and Bioengineering (NIBIB), these two groups worked together to create the two female phantom crew members Helga and Zohar aboard the Orion spacecraft. They were launched into space Nov. 16 for a 42-day flight around moon and back to test the spacecraft, and more importantly, the safety of radiation protection of the ship and personal astronaut shielding.
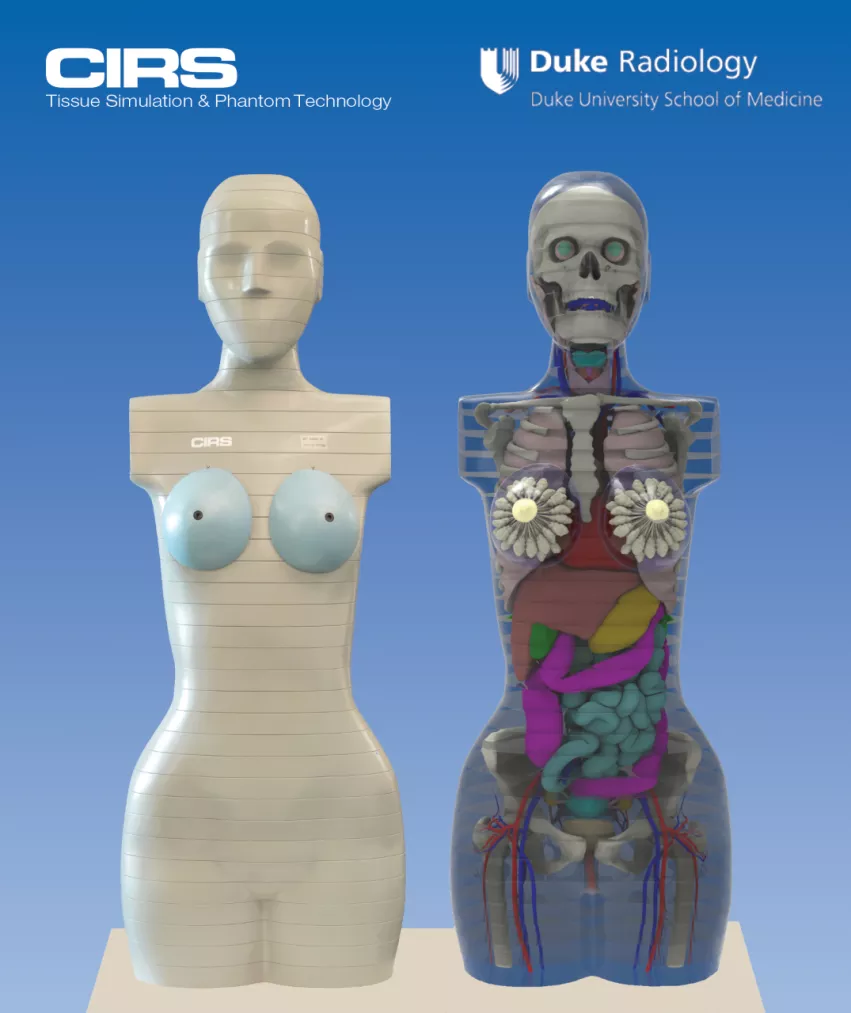
Phantoms are used by medical physicists in hospitals to quality assurance test (QA) X-ray, computed tomography (CT) angiography and radiation therapy systems to check that doses the systems emit are actually what is being received in the phantoms. Phantoms can be quite sophisticated and the materials are carefully calibrated to match actual human tissues.
"Our center has been in the process of creating human models for imaging or radiotherapy applications, so for years we have been creating human models with internal organs," Samei explained. "When this project came about, there was a need for these types of phantoms to be shipped around the moon. We collaborated to create a GPS of the organs so we would know how much radiation was received by the different organs. The two phantoms are filled with thousands of sensors so we can measure the radiation dose to different organs."
One of the phantoms has a shielding device and the other one does not, so the experiment will have a control.
"The question we are trying to answer is if that shielding device is effective and how effective is it," Samei said. "In deep space there are a lot of cosmic rays, and if we have a Mars mission that would take months or years, the question is, how much radiation burden would there be to the astronauts? It was great to be able to see our technology used in this way. This is the first time we have been able to send into deep space two full-size and full-weight human models so we can assess the radiation burden so precisely for astronauts."
Missions to the moon and beyond to Mars will take humans outside of the atmosphere and the Earth's strong magnetic field, which protects us from harmful levels of radiation emitted by the sun and other cosmic sources. The Artemis II and further manned missions will take humans outside of Earth's radiation protection for long periods of time, and it just is not known how cosmic rays will impact astronauts or cause health issues. For a mission to Mars, while we have the technology to physically get a human there, there are still questions if a human could survive such a mission if they are exposed to high levels of radiation of an extended period of time. That is why this phantom experiment is likely the most expensive, but also very important part of future deep space exploration.
The phantoms on the Artemis mission were constructed by the vendor CIRS, now part of Sun Nuclear, which makes commercial medical phantoms for calibrating radiation dose on imaging systems and radiation therapy systems. Samei said materials used to make the phantoms and the organs inside all match the density of real human tissue so that accurate measures of radiation exposure can be assessed. This technology has been used for years on earth to ensure patient safety and quality assurance on imaging and treatment systems.
"Different organs have different radio sensitivity, so if you want to get a gauge of the actual radiation burden, you you need to know how much radiation was received at specific locations inside the models,"
The radiation dose telemetry data will not be known until the Artemis space capsule returns to earth Dec. 11. Samei said it will likely take a week or two before the phantoms are returned to the lab for assessment.
Why are two female phantoms on the Artemis mission?
Samei said this experiment uses female phantoms because the female anatomy is more sensitive to radiation exposure than the male anatomy. He said exposure estimates for male astronaut radiation exposure can be calculated from the female phantom data. The assessment of the data and the use of phantoms, he added, is very much like normal assessments of medical radiation.
“With enough realism, you can do medical experiments to figure out whether an intervention is effectual or not by trying it on a computational model,” Samei said. “When we are exposed to radiation, the damage is deposited directly into the organs, and different organs have different levels of radiosensitivity. For example, breast tissue tends to be more radiosensitive, while muscles are not as radiosensitive. The brain is less radiosensitive than the heart. That’s why it is essential for the study to keep track of radiation and where in the body it is deposited.”
The Artemis I mission is the first step in NASA’s plans to carry human crews to further explore the lunar surface and eventually establish a sustainable outpost on the moon. The flight would also contribute to the groundwork required for a mission to Mars.
Additional coverage of RSNA 2022 is available here and here.