Federal law change would require all insurers to cover any supplemental breast imaging
U.S. House lawmakers are proposing a bill that would require all insurers to cover any supplemental breast imaging, beyond screening mammograms, with no patient out-of-pocket costs.
The Find it Early Act would apply to private payers, along with traditional Medicare and Advantage plans, Medicaid and TRICARE. Introduced by Reps. Rosa DeLauro, D-Conn., and Brian Fitzpatrick, R-Pa., the bill has drawn support from several patient and provider advocacy groups, including the American College of Radiology.
Journalist and breast cancer survivor Katie Couric also is throwing her weight behind the effort.
“We must strengthen access and coverage for additional testing, specifically for women like me with dense breasts,” Couric said in an announcement from the two lawmakers. “Breast cancer is treatable, and 99 percent of women who are diagnosed early survive. That is why everyone needs to get screened. The Find It Early Act is a critical step toward improving access to these life-saving screenings.”
In the wake of the Affordable Care Act, insurance carriers are required to cover screening mammograms. However, women at high risk for the disease or with dense breast tissue may sometimes require additional testing via ultrasound or MRI. Numerous analyses have charted challenges arising from women having to pony up when their insurer won’t cover these exams. A March study including nearly 231,000 commercially insured women found that individuals faced with higher cost-sharing received significantly fewer subsequent procedures.
DeLauro and Fitzpatrick also previously proposed the Find it Early Act in December, but it failed to find passage. Others voicing their support this time included DenseBreast-info, the Brem Foundation to Defeat Breast Cancer and the Susan G. Komen organization. Absent any federal action, several states have proposed bills to address insurance coverage gaps in breast cancer imaging.
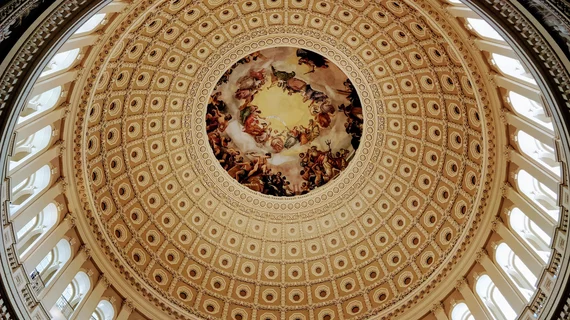
H.R. 3086 was reintroduced on May 8 at the start of the American College of Radiology’s Annual Meeting in Washington. More than 450 radiologists advocated for the bill—along with the recently reintroduced FIND Act—as part of ACR’s 2023 Capitol Hill Day.
“ACR's Government Relations team was encouraged by the late-breaking action and continues to monitor and advocate on these bills,” the college said in a Friday, May 19, news update.