Combining DXA, quantitative CT makes for most effective osteoporosis diagnosis
Combining a traditional approach to osteoporosis screening with quantitative CT starting at age 55 could reduce a woman’s lifetime risk of hip fracture while offering a cost-effective route for prevention, according to a virtual study published in Radiology this month.
Osteoporosis costs the U.S. two million broken bones and an estimated $17 billion in healthcare funds each year, lead author Christoph A. Agten, MD, and colleagues wrote, yet its gold standard for detecting and diagnosing the condition—dual-energy x-ray absorptiometry (DXA)—is often ineffective.
“The major limitation of DXA is that its use for detection of increased fracture risk is poor in the majority of individuals,” Agten, a radiologist at Balgrist University Hospital in Zurich, Switzerland, wrote. “Most patients with fragility fractures do not meet the DXA criterion for osteoporosis.”
In their research, Agten et al. sought a solution that could diagnose osteoporosis more effectively without breaking the bank. The team ultimately combined conventional DXA with quantitative CT beginning at 55 with follow-up CTs every five years—a model that would cost between 10 and 12 times more than DXA alone, but that Agten and co-authors said would actually save money by preventing further injuries down the line.
The researchers used TreeAge Pro modeling software to build a virtual, hypothetical cohort of one million post-menopausal women, according to the study. The patients, all of whom had risk factors for fracture, cycled through various life stages including fracture, no fracture and death. If they met existing criteria for osteoporosis, the women were assumed to be undergoing treatment with oral bisphosphonates.
Comparing the effectiveness of either no screening, screening with DXA alone or a combination of DXA and quantitative CT, Agten and his team found that the combined approach not only lowered a woman’s lifetime risk of hip fracture to 12.8 percent, but also proved the most cost-effective method.
That risk assessment compared to an 18.7 percent lifetime risk of hip fracture for women who skipped screening altogether and a 15.8 percent risk in those who were screened using DXA alone.
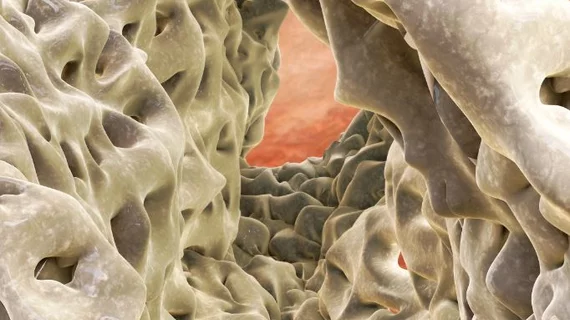
“It takes quite a lot of bone loss before you can detect a difference in bone mineral density, but the trabecular bone network can change orientation or get thinner, decreasing the structural strength of the bone,” Agten told the Radiological Society of North America. “The bone strength test, or the bone microarchitecture analysis, provides information we do not get using only DXA.”
Preliminary results are promising, Agten said, but clinical trials are necessary.
“Those findings were quite reassuring,” he said to the RSNA. “It could have been the other way around, that every strategy had the exact same amount or proportion of the best results.”