Terms of Patient Engagement: Insights From Practices Pursuing Stronger Relationships with Patients Across 4 Care Settings
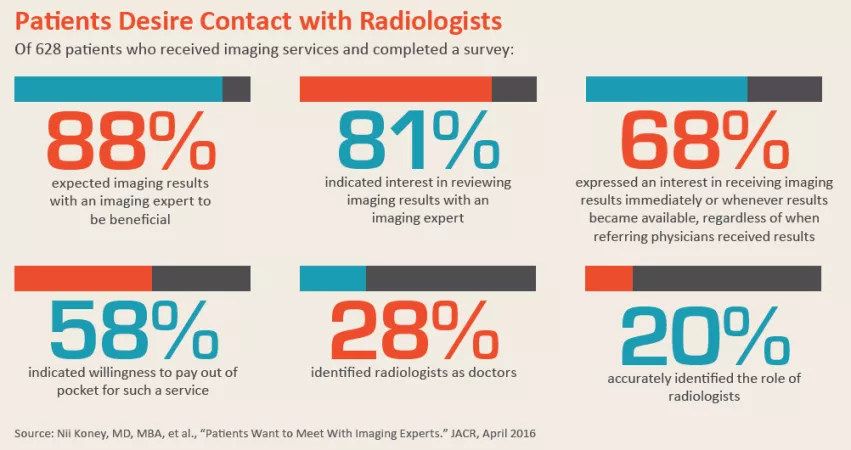
Diagnostic radiology has seen patient engagement grow, over the past few years, from an “as time permits” nicety into an out-and-out necessity. Not only is reimbursement staked to patient satisfaction more than ever before—have you checked your HCAHPS patient-satisfaction scores lately?—but many patients and radiologists want more interaction with one another, too.
This past January, new research underscored the evolution. The American Journal of Roentgenology published a survey-based study conducted by Sheila Mohan, MD, and colleagues at Emory Healthcare. The team found that 96 percent of cancer patients at a busy clinic who went over their results with a radiologist found the consultation helpful. Almost as many, 93 percent, said they’d like to review future studies with a radiologist.
And in JACR, Olga-Rachel Brook, MD, of Harvard and colleagues reported that most radiologists surveyed at their institution, some 78.7 percent, said they found interactions with patients to be a satisfying experience. More than half, 54.3 percent, further expressed a desire for expanding opportunities to interact with patients.
What does the uptick in radiologist-patient engagement look like on the ground? In most cases it involves some combination of digital and face-to-face contact. That’s one thing RBJ heard more than once when we spoke by phone with radiology folks applying focused patient-engagement strategies in four practice settings. Here’s a sampling from each.
Academic Medical Center:
The Efficiency Paradox
“My imaging practice has always included a great deal of robust interaction and communication with referring physicians about their patients—and lots of direct communication with patients.” So says Laurie Loevner, MD, division chief of neuroradiology at the University of Pennsylvania Health System. “Every day, I speak to many long-term patients. They call my cell, they text me, and I often meet them in person if it’s bad news or great news.”
Colleagues ask her if patients abuse the privilege having her cell number. “Most patients respect your time,” she says. “Few overstep the boundaries.” Being close to patients, she says, has led hundreds to choose her as the radiologist who cares for them on an ongoing basis—a relative rarity in radiology.
When she has a patient who received care outside of Penn Medicine and who arrives with gaps in his or her EMR, Loevner often calls that patient directly. Connecting with the referring doctor in the middle of a busy day can be difficult, she says, adding that once the patient is on the line, she doesn’t hesitate to explain radiology’s role in patient care.
Loevner, a professor of radiology, ophthalmology and neurosurgery, has been training young doctors for years to engage closely with patients. She says such engagement, paradoxically, increases workplace efficiency over the long haul.
“I remember patients’ prior images without having to retreat to study them before reading their next follow-up imaging study,” says Loevner, who reads imaging exams for around 150 patients per week. She maintains that she can interpret one of her long-time patients’ studies in a matter of minutes, where a radiologist unfamiliar with a patient might need significantly more time.
Loevner usually schedules clinical imaging days on Mondays and Tuesdays. Her patients know, and many line up their tests accordingly. She encourages other radiologists to try her approach, warning that there will be a steep learning curve.
“It is a paradigm shift,” she says. “But when you start getting returning patients and you know their stories inside out and you know them as human beings, not only will you be more efficient, but the real reward is the patient-doctor interaction.”
Meanwhile the numbers speak volumes. Penn Health’s neuroradiology department is projected to log 169,000 RVUs this year. That’s an increase of 19 percent over 2017 (141,758 RVUs) and of more than 26 percent over 2016 (133,531 RVUs).
But for Loevner, building and maintaining close relationships with patients delivers less quantifiable but equally rewarding returns: It brings her joy, she says.
“The patients genuinely appreciate it,” she says. “They consider me their doctor. And the clinicians recognize my expertise with the patient. It’s a win-win-win.”
Community Hospital:
Referrer Buy-In at 99%
At the Sheila R. Veloz Breast Center, which is a part of 238-bed Henry Mayo Newhall Hospital in Valencia, Calif., a patient whose diagnostic mammogram reveals a suspicious finding immediately speaks with the radiologist who made the finding.
“The radiologist will often bring the patient into the reading room and show her the images and explain what they’re looking at,” says Terry Lynn Bucknall, director of women’s imaging services.
If a screening exam raises concerns, the patient may also have a diagnostic workup on the same day. That may include additional mammography images, an ultrasound and possibly a core needle biopsy. A radiologist will also discuss the findings with the patient as she or he moves through the diagnostic process that same day.
“If something looks suspicious, the radiologist will try to alleviate the patient’s fears,” says Bucknall, adding that great care is taken to very gently convey the need for speed. At the same time, to expedite the testing processes when lesions are found, the center encourages referring physicians to write initial orders granting the radiologist permission to perform additional needed tests.
“Our patient navigator has communicated with our referring physicians about [greater radiologist involvement], and 99 percent of them have agreed” that it’s a good thing, says Bucknall.
The goal is to eliminate avoidable delays. In the past, Bucknall says, these occurred fairly often when the call for next diagnostic steps only came from the referrer.
“We were finding that many of the referring physicians were not following through on a timely basis or not doing it at all,” says Bucknall. “Some referring providers are not educated or comfortable discussing breast imaging with their patients. They prefer to leave it to the ‘experts.’”
The Veloz center occupies its own office in an outpatient building near the hospital and contracts with four radiologists who specialize in breast imaging. One of the radiologists is present and available to speak with patients each weekday. The center also has evening and weekend hours. At those hours, a radiologist isn’t always present for immediate patient discussions.
“We are in the process of improving our services, which may include extended hours for our radiologists,” says Bucknall.
Radiologists who specialize in breast studies can better explain images and findings to patients than most referring physicians, suggests Bucknall, adding that the Veloz center is the only dedicated women’s imaging operation in its area. “An MD who specializes in internal medicine is not an expert at explaining breast imaging,” she says. “They don’t know the details.”
As for connecting focused patient engagement with good business performance: The center is relatively small, yet it serves around 12,000 patients per year, performing 14,000 exams. Some 9,500 of these are screenings, and the center has averaged 42 cancer detections at screening over the past three years. Not surprisingly, patient satisfaction scores, Bucknall reports, are “very high.”
Private Practice:
The Digital Difference
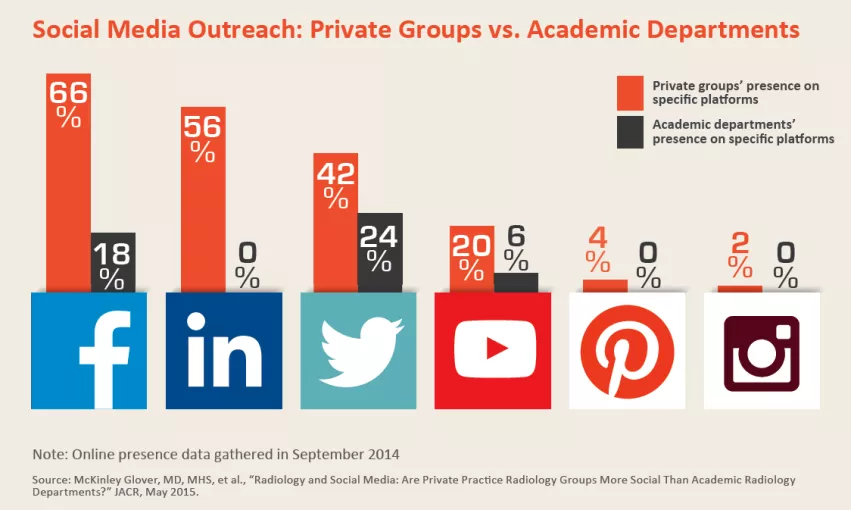
Members of the Millennial generation are now in their 30s. This means they’re either already in or quickly approaching the stage of life in which annual screenings become a thing, points out Kyle Baril, a marketing specialist with Radiology Ltd., a large private practice in Tucson, Ariz.
Millennials, he continues, “demand a lot in the way of online patient communication.” They essentially live online, he says, and are ready, willing and able to get to know their doctors via smartphones, tablets and laptops.
That acknowledged, Baril says he would love to see more in-person contact between radiologists and patients. “To build that relationship, it’s really important to connect a face with the name of your doctor,” not to mention a voice and a handshake.
As a way to bridge the divide, Radiology Ltd. has begun recording videos in-house and posting them on its website. The videos on offer focus on educating patients about imaging procedures and technologies. To these the practice may add brief autobiographies or greetings from individual radiologists, Baril says.
Either way, the videos “make the radiologists human,” Baril says. “They’re not just robots in a dark room.”
Affordability is not the only challenge in creating the videos in-house. “If you do the videos wrong, the project can backfire and you can actually lose credibility,” says Baril. The success of the video series depends heavily on the doctors’ on-camera personalities, along with their ability to speak simply and engagingly.
“The biggest challenge for us is doctor-speak,” Baril says. “The doctors use a lot of inside terminology.” Meanwhile, to be successful in reaching patients, he says, videos need to target people who read at just a fourth-grade level.
“If you can do the videos professionally and the doctor comes off well, this can be a game changer,” says Baril. If, however, the physicians do not seem approachable in the recordings, videos simply may not work, he says. “Not every doctor is going to be comfortable in front of the camera.”
In addition, the practice’s website includes a quick self-assessment that visitors can take to see which preventive screenings might be suitable for them, based on factors such as age, lifestyle and family history. So far, more than 1,000 people have completed the self-assessment. And last year Radiology Ltd. performed 566,000 exams, Baril says, adding that this made 2017 one of the practice’s best years ever.
VA Hospital:
Long Waits Busted
For Donald Perry, MD, it was specifically the desire to interact with patients that led him to choose interventional radiology as his specialty. “I still try to speak with every patient I care for,” says Perry, who until July 2017 was affiliated with the Veterans Affairs (VA) Puget Sound Medical Center in Seattle. Currently he practices with Radiology Specialists of Florida and serves as assistant director of the radiology residency program at the University of Central Florida.
To describe his idea of a patient-centered approach to diagnostic radiology, Perry uses the example of a patient with an esophageal mass.
“The old way, a patient would see his doctor complaining of difficulty swallowing. Then the patient would come to us,” he says. The patient may have an ultrasound, an x-ray, fluoroscopic exam or a CT scan looking for an obstructing mass, narrowing or other cause of the patient’s symptoms, he continues. Then the patient would go home, and the radiologist would dictate a report about the imaging results for the referring doctor.
“Say the imaging was done on a Friday. Maybe the ordering provider sees the results on Monday or maybe later,” Perry says. “Meanwhile, the patient is sitting at home with the same symptoms, waiting for a diagnosis.” Eventually, the referring physician would call the patient and tell him to go see a gastroenterologist for an endoscopic exam or perhaps a biopsy.
Instead of taking that approach, at the VA, when the technologist or radiologist noticed that kind of finding, the radiologist would call the referring physician, Perry explains. “The radiologist will say, ‘I have your patient with dysphagia here. He has an esophageal mass and I am going to make a referral to a gastroenterologist.’ And the referrer will say, ‘Yes. Let’s get it done.’ The radiologist then helps them order a staging CT of the abdomen.”
The patient-centric approach brings many advantages, says Perry. “It hastens diagnosis and clinical workup. It reduces the workload overall and the utilization of resources that a patient consumes,” he says. It also saves the patient time and shortens the period of anxious waiting for a decisive diagnosis.
Perry acknowledges that reimbursement issues pose challenges. “Any time a radiologist leaves the workstation, administration may see it as wasted time because it is not reimbursable,” he says. “If you’re a diagnostic radiologist, they would prefer you read more studies over communicating with your patient or coordinating care.”
To overcome such objections, he says, direct patient engagement should be built into the practice-management model and conducted with respect for administrative leadership’s legitimate concerns over unbillable time. Making patient engagement efficient without sacrificing care quality, Perry says, has to be “a top priority.”