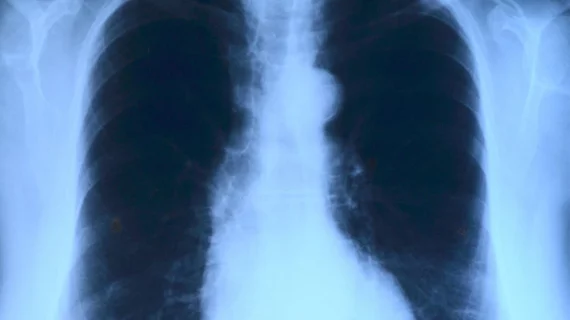
Chest x-ray algorithm much faster than experienced radiologists, but not always better
Stanford University researchers have produced a convolutional neural network (CNN) capable of finding most of 14 different disease states—nearly everything from pneumonia to lung cancer—on chest x-rays. What’s more, in a study testing the system, experienced radiologists spent an average of 240 minutes interpreting a large image set that the algorithm whipped through in just 90 seconds.
The study was published online Nov. 20 in PLOS Medicine.
Lead author Pranav Rajpurkar, a PhD candidate in computer science, senior author Matthew Lungren, MD, MPH, and colleagues trained their CNN, which they’re calling CheXNeXt, on a publicly available image dataset. They used a validation dataset of 420 images and had three board-certified cardiothoracic specialist radiologists serve as this dataset’s reference standard.
The researchers constructed the validation set to contain at least 50 cases of each of 14 pathologies.
Comparing the algorithm’s performance on the validation set to that of nine radiologists, the team found that CheXNeXt achieved radiologist-level performance on 11 of 14 pathologies.
On three pathologies—cardiomegaly, emphysema, and hiatal hernia—the radiologists soundly outperformed the algorithm.
Still, the CNN’s excellent overall performance justified its consideration for use in clinical practice, the researchers suggested.
“In this study, we developed and validated a deep learning algorithm that classified clinically important abnormalities in chest radiographs at a performance level comparable to practicing radiologists,” Rajpurkar et al. wrote. “Once tested prospectively in clinical settings, the algorithm could have the potential to expand patient access to chest radiograph diagnostics.”
The authors noted as their main limitations the use of an image dataset from a single hospital system and the withholding of patient histories and prior exam results from both CheXNeXt and the radiologists, which would not occur in clinical practice.
In their discussion, the authors considered the potential value of the tool in light of the World Health Organization’s estimation that more than 4 billion people lack access to medical imaging expertise.
“Even in developed countries with advanced healthcare systems, an automated system to interpret chest radiographs could provide immense utility,” Rajpurkar and colleagues wrote. “This algorithm could be used for worklist prioritization, allowing the sickest patients to receive quicker diagnoses and treatment even in hospital settings in which radiologists are not immediately available.”