What simulation models can teach us about treating ground-glass nodules
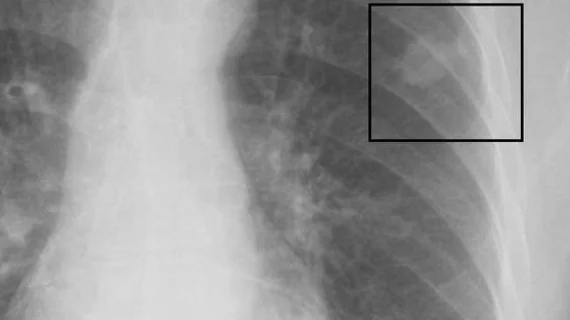
Healthcare providers should consider updating their follow-up interval for patients with ground-glass nodules (GGNs) detected on CT exams to three years, according to new research published in Radiology.
The authors developed a simulation model for 1 million patients with GGNs receiving follow-up care as recommended by the American College of Radiology’s Lung Imaging Reporting and Data System (Lung-RADS) recommendations. The mean age for these hypothetical patients was 64 years old.
The team studied how these patients would be affected by annual follow-up compared to follow-up every three years. Since questions remain about the optimal way to care for patients with GGNs, the impact of different treatment strategies—stereotactic body radiation therapy (SBRT), surgery, no therapy at all—was also explored.
Overall, 2.3 percent of the nodules were clinically significant malignancies. In addition, just 30 percent of the nodules that required treatment (Lung-RADS category 4B or 4X) were clinically significant malignancies. Overall survival (OS) at 10 years with annual follow-up was 71 percent. Using three-year intervals, overall survival (OS) was 71 percent.
“Our results suggest taking a conservative approach to the follow-up and treatment of GGNs,” wrote Mark M. Hammer, MD, department of radiology at Brigham and Women’s Hospital in Boston, and colleagues. “While there is a high rate of malignancy in these nodules at biopsy, the rate of clinically significant malignancy is lower, and, overall, these malignancies demonstrate an indolent course. Our results argue for raising the follow-up interval for GGNs to three years.”
The authors also found that OS among patients with nodules that required treatment was 80 percent after SBRT, 79 percent after surgery and 74 percent after no therapy. These statistics, they wrote, “suggest the use of treatments that incur less morbidity (eg, radiation therapy) when a nodule has met criteria for treatment.”