Virtual Hearts in Actual Hands: Medical 3D Printing Polishes Its Act for Prime Time
Medical 3D Printing Polishes Its Act for Prime Time
The surgeon repairing the tiny infant heart knew he faced a daunting task. He’d have to work on the delicate organ and vessels hindered by limited access routes for observation. And the rarity of the baby’s congenital defect would force him to draw on surgical skills he hadn’t yet developed.
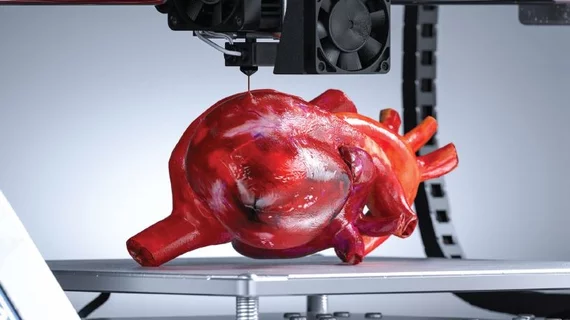
This time, though, the physician averted the apprehension he’d normally experience when one wrong move might risk the life of a patient just a few months old. For the heart in his hands belonged to no live human infant: It came to the surgeon as a 3D printed model made of a flexible, lifelike material.
The no-risk, hands-on training equipped the surgeon with a clear and precise anatomical fix on procedures like closure of the septal defect, reconstructing the aortic arch and performing an arterial switch. It gave him a practice run grounded in not only in visual precision but also tactile response.
Those who’ve trained, planned and practiced with the technology will say with one voice that no image on a computer screen, regardless of its level of advanced visualization, could match medical 3D printing’s combination of sight and feel.
“It’s made a small revolution in teaching and surgical practice,” says Shi-Joon Yoo, MD, PhD, of the highly successful 3D printing training program for congenital heart surgery he created at the University of Toronto’s Hospital for Sick Children. (Check out the program’s doings at 3dprintheart.ca.)
“3D printed models are proving to be a tremendous resource,” says Yoo, a professor of medical imaging. “They represent the future of surgical training.”
Roads to Reimbursement
Typically originating from 3D volume-rendered image data of a patient's CT or MRI or echocardiography, three-dimensional printed models are capturing the imagination of more and more surgeons, proceduralists and radiologists.
And the enthusiasts’ numbers are certain to continue growing. These graphic anatomic replicas are now used mostly for preoperative planning, intraoperative guidance and medical trainee education. However, in coming years, the technology will evolve into bioprinting, which lays down a cellular scaffolding for an unlimited and cost-efficient supply of custom implants, prostheses, body tissue and organ-like constructs.
The current reality is a bit more earthbound. Before 3D printing can become anything approaching a groundswell in the medical community, some significant hurdles must be cleared.
For one thing, 3D printing represents a substantial investment. (See accompanying article “3D Printing: Costs to Consider".) Hospital and department heads must be convinced of its cost-effectiveness, as well as its ability to draw the interest of surgeons, before making the leap.
The highest hurdle, though, can be summed up in a word: reimbursement, of which there is very little at present.
That calculus could soon be changing. This spring a new 3D printing clinical data registry is scheduled to go live. A joint project of RSNA and ACR, the registry is designed to collect 3D printed data at the point of clinical care to document the technology’s use, value and implementation.
In addition, the American Medical Association has approved the creation of four Category III CPT (Current Procedural Terminology) codes governing 3D printed anatomic models and surgical guides. The AMA approval came in November 2018 and the codes took effect July 1, 2019.
These temporary tracking codes are part of a stepwise process expected to lead to adoption of Category I CPT codes and widespread reimbursement.
Hurry Up and Wait
For now, though, 3D printed anatomic models may not be covered by CMS or third-party payers. And the kind of large, randomized trials needed to provide the supportive evidence insurers demand are generally lacking.
That’s why CPT codes and the fledgling data registry are tightly linked—and critical to the future of 3D printing as an accepted part of clinical practice.
“When we apply later for Category I codes, we will need peer-reviewed documentation, and that is where the [ACR/RSNA] 3D printing data registry comes into play,” says radiologist William Weadock, MD, of the University of Michigan Medical School. He serves as the 2019 chair of RSNA’s 3D printing special interest group, which is leading the charge toward code enactment.
“Through a nationwide registry we’ll be able to show what people are doing in terms of different cases and applications, materials and actual prints,” Weadock adds. “In short, the registry will supply the data needed to benchmark the value of this very promising” medical technology.
How long before Category I codes open the reimbursement spigot? Weadock and other experts concede the development process is slow, saying stakeholders should expect to wait another two to four years.
3D Economics
One recent study, however, has given the pro-reimbursement forces a considerable boost.
Designed to provide an economic rationale for 3D printing in orthopedic and maxillofacial surgical applications, the study, based on a review of other analyses, found that anatomic models can shorten operating room time by 62 minutes, on average, for a total of $3,720 per case, and that 3D printed surgical guides saved an average of 23 minutes of OR time, for a total of $1,488 per case.
What’s more, the study, published online last September in Academic Radiology, showed that, by printing an estimated 63 models or guides a year—a rather modest output—users could break even and account for their annual fixed costs.
These findings led the researchers to conclude that 3D printing “has the potential to pay for itself.” The authors note that worthwhile “payments” would include value-adds like “superior confidence of the surgeon or proceduralist, the ability to perform complex procedures that were poorly understood anatomically with 3D visualization and financial savings secondary to shorter, more efficient procedures.”
The study’s lead author, David Ballard, MD, a fourth-year radiology resident at the Mallinckrodt Institute of Radiology in St. Louis, believes his team’s analysis is especially pertinent to technology selection and purchasing teams stuck on the fence over 3D printing.
“We hope the metrics from our study can serve as a tool to be presented to [hospital] administrations and leaders,” says Ballard, a member of RSNA’s 3D printing special interest group. The study plainly showed that surgical time saved “can be substantial, in the thousands of dollars per case,” he says. “It’s becoming clear that, while they’re resource-intensive, 3D printed constructs used in patient operative care can provide considerable downstream value to health systems.”
Shaving Time
A telling snapshot of the present and future of medical 3D printing is there for the observing in 34 Veterans Affairs hospitals around the country.
According to Beth Ripley, MD, PhD, a VA Puget Sound radiologist in Seattle who chairs a committee advising the entire Veterans Health Administration on 3D printing, 3D printed replicas of TAVR valves, for example, are now being used by interventionalists prior to performing these minimally invasive yet intricate procedures at those 34 locations.
“We print a section of the heart, the faulty valve and all the anatomy surrounding where the heart valve will go,” Ripley explains. “This gives the interventionalist—who previously could only visualize the landscape through two-dimensional radiography or fluoroscopy—a handson opportunity to figure out all the challenges and try out different size valves beforehand. They can make sure they have the right fit for the patient's heart.”
The opportunities are now expanding to mitral valve repair. VA Puget Sound Health Care, which has teamed up with the University of Washington to create some 300 heart models over the past year, is starting to print physical constructs for mitral valve repair that leave nothing to the imagination.
The aorta and heart wall are printed from an elastic, malleable material that behaves like the heart, while calcifications that impact the landing of the valve are simulated from a hard material that mimics how the anatomy will interact with the valve once it’s situated in the model. The complex fabrication takes about four hours to print.
But that process could soon accelerate dramatically. This past November, VA Puget Sound announced a partnership with a major healthcare technology vendor that could compress the time it takes to create 3D models from hours to mere minutes.
“With just a few clicks, we’ll be able to get to the part of the anatomy we need for our model,” Ripley says. “That will enable us, for example, to segment the spine and associated intravertebral discs in as little as five minutes. That process now takes up to an hour.”
Bioprinted Body Parts
The next major frontier for medical 3D printing developers to conquer may be bioprinting.
While individually designed, 3D printed organs like the heart, lungs or kidney once seemed more sci-fi than bio-sci, they could now be just years away. Tissue engineering that allows for 3D printed cardiac valves, skin, ear and eye implants made from patients’ own stem cells—thus reducing the risk of rejection and conferring the ability to grow with the patient—is on the near horizon. And 3D printed prosthetic hands, arms, feet and legs are already on the market.
The prospect of creating the bioequivalent of something as simple and basic as a small piece of human bone has scientist/clinicians roused into envisioning the possibilities. Ripley, for one, weighs the immense potential against the current reality of complex fractures that never heal. Sometimes that’s the case for patients with tumors of the jaw or mandible that have to be cut out and replaced by bone taken from the leg.
“Imagine if we could just create a small section of bone that’s living, matches the defective section and could be implanted in the patient,” she muses. “It could be a game-changer.”
Weadock states his eager anticipation of good things to come this way: “The human body is ripe for 3D printing applications. And there are lots of innovative people out there who are going to figure it out.”
Ready, Radiology?
Of course, 3D printing is not yet on every clinician’s radar screen. It’s not even close. And without strong support from surgeons and radiologists alike, an institution is unlikely to move forward with a dedicated, adequately resourced program.
“At our institution, it seems to be somewhat of a generational thing, with younger surgeons more open to changing their practice by using 3D printed models,” says Ballard at Mallinckrodt Institute of Radiology, which maintains an active 3D printing program. “But the small number of surgeons I’ve been in contact with are very excited about the prospect of using them, or having their attending surgeons or trainees use them, for visualization and education.”
Ripley recounts the case of one VA surgeon who was less than totally satisfied with the models she was creating for him because “he didn’t feel I understood what his challenges and questions were.” So she scrubbed in for a case, and that proved to be the radiologist’s epiphany.
“Now I create models that focus more on landmarks such as the blood vessels he needs to avoid as he works his way toward the kidney and tumor,” she explains. “He needed models showing him how to get there faster and safer, rather than showing him what he would see when he arrived. He got them, and now he loves them.”
Like their colleagues in surgery, many radiologists continue to question what they stand to gain from the adoption of an unproven technology that takes them outside their comfort zone. The message for resisters from those with experience in the field is decidedly encouraging.
“As we’ve become more digital, the number of visitors to the radiology reading room has become fewer,” Ballard points out. “3D printing is an exciting new service that could reconnect us to surgeons and proceduralists, even patients. It has the potential to produce more efficient surgery and better clinical outcomes. And let’s not forget it’s something radiology as a field is uniquely poised to do.”