Transplanted lungs react to COVID in a distinctive way
Clinicians treating COVID-19 patients who have transplanted lungs and lower airway infection should order molecular testing in addition to, or regardless of, imaging findings.
Researchers in the U.S. and Brazil make the recommendation after reviewing the cases of 51 consecutive lung transplant recipients and 75 controls, all of whom were hospitalized with COVID at one of two centers.
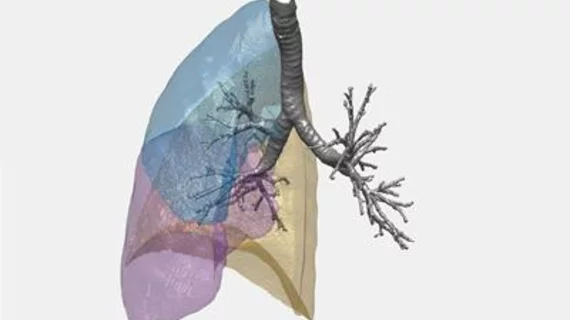
Radiologist Bruno Hochhegger, MD, PhD, of the University of Florida in Gainesville, pulmonologist Douglas Nascimento, MD, of Santa Casa de Misericordia Hospital in Porto Alegre and colleagues further found the transplant recipients tend to show predominating lung consolidation as their most common CT finding.
By contrast, the controls had predominating patterns of ground-glass opacities.
European Radiology published the team’s study online Sept. 24.
“The imaging findings of COVID-19 in lung transplant recipients were significantly different from controls regarding the RSNA classification and pattern of lung attenuation,” the authors remark [1]. “Lung transplant recipients had a significantly higher proportion of patients with an indeterminate pattern on CT.
They further found the second most common attenuation pattern in the transplant patients was a mix of ground-glass opacities and consolidation.
Also, the transplant recipients had significantly more severe parenchymal lung disease going by CT score and percentage of high attenuation areas at quantitative CT.
Ground Glass Opacities a Clear Dividing Line
The study’s patient population comprised individuals who were hospitalized for COVID-19 from July 1, 2021, to Feb. 9, 2022.
All patients had documented SARS-nCoV-2 infection diagnosed by real time reverse transcription–polymerase chain reaction (RT-PCR) and at least one chest CT performed within 48 hours of hospitalization, the authors report.
Hochhegger and co-authors observed a predominant pattern of ground glass opacities in only 23.5% of the COVID patients with transplanted lungs.
In their discussion they suggest this might be explained by the transplant patients’ immunocompromised state combined with their higher susceptibility to more severe forms of the disease with more consolidation.
Meanwhile the non-transplant controls most often presented with a pure or predominant pattern of ground glass opacities (56.0%). This is consistent with prior research into immunocompetent patients, the authors comment.
Molecular Testing a Must
Hochhegger and co-authors underscore that the higher frequency of indeterminate COVID patterns in the transplant recipients “highlights the importance of molecular testing for COVID-19 in immunosuppressed patients presenting with lower airway infection.”
As for COVID mortality in lung transplant recipients, the authors note that previous studies, most of them retrospective, have found it spans from 12% to 46%.
“Our population had reported mortality in the lower end of this spectrum, particularly because all patients were vaccinated at least twice for COVID-19,” they write. “Also, some of the other studies had mixed data from outpatient and inpatient, while others were done in more severe cases, which contributes to the wide range of the spectrum.”
More:
The timeframe of the [present] study was long, and we have not investigated how different variants of COVID could have influenced some of the findings. The primary goal of this study was to investigate the chest CT findings of COVID-19 in lung transplant recipients, and it was not designed or powered to investigate mortality in these patients. Therefore, mortality outcomes should be interpreted with caution due to high risk of bias.”
The study is available in full for free.