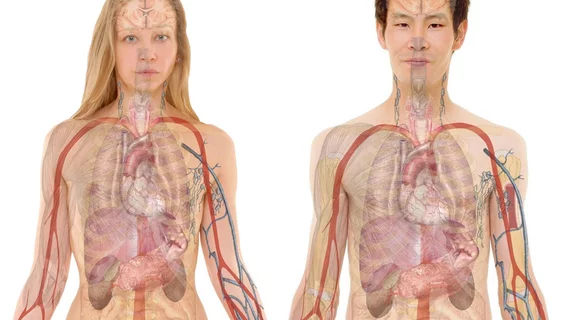
Cross-organ imaging illuminates the heart-brain-liver axis
A population-level study featuring multi-organ MRI has confirmed that problems in any of three major organs—the heart, brain or liver—tend to co-occur with unfavorable findings in either or both of the other two.
The research documents the associations persisting regardless of variables in demographics, lifestyles and environmental settings.
It also shows the cross-organ effect holding despite differences in vascular risk factors such as diabetes, hypertension, high cholesterol, elevated BMI and smoking.
The work was conducted in the U.K. and is described in a paper published Dec. 21 in Nature Communications [1].
Cardiologist Zahra Raisi-Estabragh of Queen Mary University in London and colleagues analyzed data on 14,539 men and 15,905 women in the U.K. Biobank.
The team found the most consistent markers for multi-organ disorder in these generally healthy populations were liver fibro-inflammation (liver/brain path), liver fat (liver/heart) and aortic distensibility (heart/brain).
When all three organs were implicated, direct and indirect associations were apparent with both heart and liver for brain outcomes such as smaller gray matter volumes and greater white matter hyperintensities.
Again, these effects held even after the authors adjusted the data for confounders.
Spelling out the point of the project, the authors note that medical imaging research “provides numerous insights into the subclinical changes that precede serious diseases such as heart disease and dementia.”
The opening for the present work arose from the observation that most imaging research either focuses on one organ system per project or analyzes data from small population samples, they state.
Moreover, “while there is now extensive evidence that heart, brain and liver disease outcomes are empirically linked, the underlying mechanisms are not well understood.”
Based on the strength of its numbers, Raisi-Estabragh and co-authors write, the present study “describes a potentially cumulative burden of multiple-organ dysfunction and provides essential insight into multi-organ disease prevention.”
More:
Looking to the future, an understanding of multi-organ interdependence is fundamental to population-level risk stratification and disease prevention, since the detection of abnormalities in any of the three organs signals an opportunity to intervene earlier in patients and alter the trajectory of disease development. … [T]he cumulative potential insights from multi-system imaging are expected to have a major impact on our ability to predict and prevent complex diseases, and reliably improve quality of life and overall survival.”
The study is available in full for free.