8 trends in radiology technology to watch in 2023
Here is a list of some key trends in radiology technology from the editors of Health Imaging and Radiology Business that clinicians should be aware of heading into 2023. These are observations they made covering radiology news on a daily basis, interviews with key opinion leaders and covering the Radiological Society of North American (RSNA) annual meetings.
Radiology AI adoption
Artificial intelligence will rapidly be deployed across medical imaging to help augment techs and radiologists so the existing staff can do more with less. AI will speed exam throughput, reduce retakes, improve image quality, help reduce dose, and help organize and pull data on the IT side to speed pulling priors, auto complete of structured reports and automated measurements. AI will likely go a long way toward helping address physician burnout and help offset some issues with radiologist staff shortages.
For more:
VIDEO: Radiology AI trends at RSNA 2022
VIDEO: Where will radiology AI be in 5 years? — Interview with Keith J. Dreyer, DO,
Movement to web-based enterprise imaging systems
Web-based enterprise imaging systems are replacing traditional PACS, where siloes between modalities are eliminated and clinicians can access images and reports from anywhere without the need for specific workstations. Access to AI and advanced imaging tools will be fully integrated into these systems and the data will interface mostly seamlessly with EMRs. This will enable greater access to images and reports across health systems and enable sharing with patients.
For more:
VIDEO: KLAS shares trends in enterprise imaging and AI
Movement to off-site cloud storage
Cloud-based archive storage by third-party server farm firms like Google Health, Amazon and others are quickly becoming the way of the future for storing images and patient data. Hospitals are realizing it is easier and possibly less expensive to outsource to companies with 24/7/365 monitoring by cybersecurity teams and the ability to upscale server storage without the need to install more hardware, cooling systems and utilizing physical space. This also allows hospitals the ability to scale storage to their needs quickly. Hospitals no longer want to house large IT storage areas, support infrastructure or devote staff to maintain these servers when it can be outsourced more economically.
For more:
Amazon marshals partners, providers behind major move into medical imaging
VIDEO: 6 key trends in PACS and radiology informatics observed by KLAS
Photon-counting CT may replace current CT detector technology
Photon-counting CT will become the wave of the future for workhorse CT imaging systems. These systems promise to help cut dose, improve image quality and offer spectral imaging built into every exam. This enables views of datasets at any energy level, material decomposition imaging so things like calcium and iodine can be mapped and faded in or out of images to show perfusion defects and the ability to reduce or eliminate calcium blooming and see inside calcified arteries.
There are currently two photon-counting CT system cleared by the FDA from Siemens and Samsung, but other systems are in development by other key CT manufacturers, including GE HealthCare and Philips.
Find more:
VIDEO: Photon-counting CT development at the University of Wisconsin
VIDEO: CT imaging market trends and advances overview by Signify Research
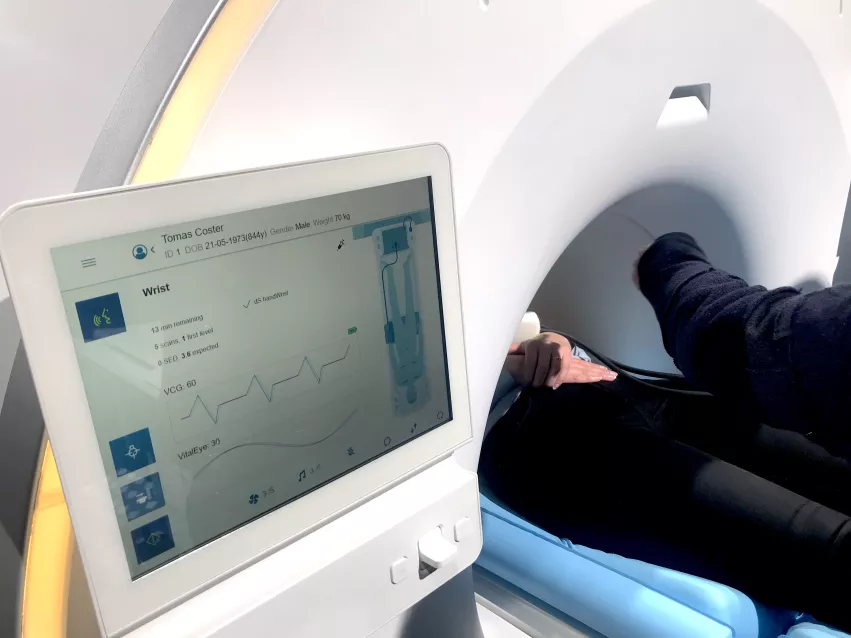
MRI is becoming easier to use and less expensive to maintain
MRI may see increased usage in the coming years due to several factors. These include AI to help setup protocols and simplify exams even with less experienced techs, speed exam times and increase the imaging protocols in a shorter exam time.
Newer MRI systems also use a fraction of helium in a sealed system to eliminate boil off and significantly cut for s to install and maintain these systems.
For more:
VIDEO: Overview of MRI market and technology trends
Top MRI trends include helium-free systems, compressed sensing and AI
3D mammography will replace standard digital mammo
Mammography is rapidly moving to 3D tomosythesis systems. According to the FDA Mammography Quality Standards Act (MQSA) data, 3D mammo systems now make up nearly 50% of the breast imaging systems in service.
While tomo adds extra read time and produces datasets that take up a lot more archive storage space, the modality is seen as a big advantage to reduce false positives, unnecessary biopsies. It also helps radiologists make better assessments because they can look through the slices of the breast tissue.
For more:
VIDEO: The rapid adoption of 3D mammography and use of AI to address dense breasts —Interview with Stamatia Destounis, MD
3D mammography approaching 50% of breast imaging systems in the U.S.
VIDEO: 3D mammography is becoming the standard-of-care in breast imaging — Interview with John Lewin, MD
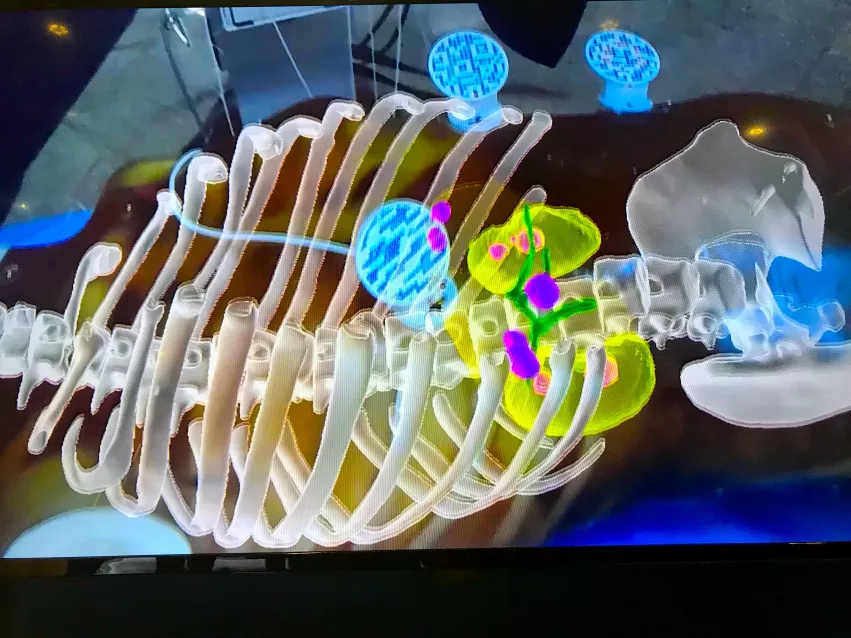
Augmented reality view of a life-like anatomical phantom fused with a CT scan 3D reconstruction of a patient's anatomy with several tumors, shown by MediView at RSNA 2022. The operator can use this view to walk around the patient and see the targets inside and use it as an aid to guide biopsies or procedures. Photo by Dave Fornell
Virtual reality aids better understanding of complex anatomy
Virtual and augmented reality (VR and AR) technology is being adopted in radiology. On the patient side, 3D medical imaging from the patient is being used for patient education about their disease or procedure.
For radiologists or other specialists, VR is being used to review complex anatomy in a virtual 3D/4D environment. This includes reviewing congenital heart disease 3D datasets and brain imaging prior to surgical interventions.
For more:
POCUS is rapidly expanding
Point-of-care ultrasound (POCUS) saw an absolute explosion of use during the COVID-19 pandemic, further extending the number of clinicians using this imaging technology. Its utility was seen by many during the pandemic and clinicians are not willing to give up this tool that enables immediate "quick-look" triage imaging.
These systems are also becoming more sophisticated in terms of image quality and measurements they can perform. This is partly due to the integration of artificial intelligence and the use of web-based computing power, so not all the functions need to reside on the mobile device being used to acquire the images.
Medical schools are starting to train students to use these devices as part of their assessment of patients, so POCUS is likely to continue to increase across all ologies. Some experts have predicted POCUS may replace the stethoscope as the standard triage tool, and it seems this may be the case over the next decade.
For more: