Palliative radiation improves life for terminal lung cancer patients—but how much is too much?
More than a third of patients diagnosed with terminal lung cancer undergo palliative radiation therapy that can improve their quality of life, but more than half of those individuals could be experiencing overtreatment, researchers reported this month.
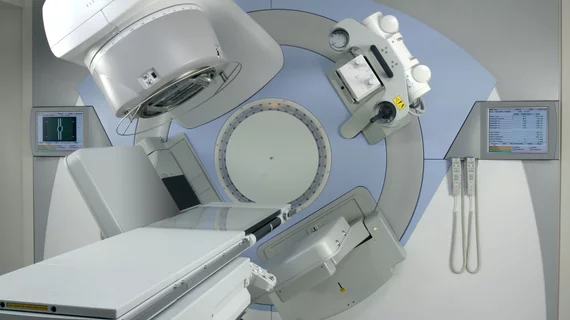
Palliative radiation therapy is a standard course of treatment in patients with incurable non-small cell lung cancer, because those patients are often focused more on prolonging life comfortably and less on a cure, Miranda B. Lam, MD, and colleagues wrote in Advances in Radiation Oncology. But the palliative approach, which typically focuses on the brain, thorax and bone, could be one that’s utilized inefficiently.
“Despite its ability to stabilize or improve symptoms, prior studies have shown significant variation in the use of palliative radiation therapy, ranging from 31 percent to 66 percent of patients with incurable disease,” Lam et al. wrote. “Even in instances when palliative radiation therapy is employed, RT fractionation schemes vary and are not always well supported by randomized data.”
In patients like those with incurable lung cancer, shorter-term radiation therapy is generally the preferred route, the authors said. Though one meta-analysis found that higher-dose radiation therapy schedules were linked to minor improvements in symptom control and survival, those developments came at the cost of increased short-term side effects, and the American Society for Radiation Oncology has actively recommended against extended fractionation schemes.
“Because the use of extended radiation therapy courses is associated with increased cost of care and is inconvenient for patients with significant disease burden and limited life expectancy, it is critical to understand the factors influencing their use,” Lam et al. said.
The researchers retrospectively analyzed data from 55,258 non-small cell lung cancer patients who were enrolled in the National Cancer Institute’s Surveillance, Epidemiology and End Results—or SEER—Medicare database. The team studied the factors associated with opting for palliative radiation therapy, as well as fractions used in treatment.
Lam and colleagues found that among the tens of thousands of study patients with terminal lung cancer, 56 percent of the group received therapy in more than 10 fractions. This is inconsistent with national guidelines, the authors wrote.
“Over 50 percent of non-small cell lung cancer patients received more than 10 fractions of palliative RT, including 42 percent of patients receiving radiation therapy associated with a bone metastasis diagnosis code,” they said. “This is consistent with findings from other studies and suggests that there may be opportunities to streamline or consolidate care by implementing programs to evaluate whether and when shorter courses of radiation are appropriate.”
The team also found that factors like younger age, female sex, chemotherapy use, being married and having a lower modified Charlson comorbidity score meant a patient was more likely to undergo conventional radiation therapy. Some of those facets, though, including gender, comorbidities and marital status, seemed to have little influence on the fractionation schemes.
The strongest predictor of whether a patient would undergo more than 10 fractions within radiation therapy came from the practices themselves, Lam and co-authors wrote. Patients treated at a freestanding radiation therapy facility, rather than at a hospital, were 1.74 times more likely than their counterparts to receive extended fractionation. Patients who underwent any chemotherapy were about 1.79 times more likely to go that route, the researchers said.
“While there are potential clinical scenarios when extended fractionation may be warranted, in most palliative settings, radiation treatments can safely and effectively be given in 10 or fewer fractions,” Lam and colleagues wrote. “Further research into the underlying factors, including potential financial incentives, that shape treatment decisions will allow for development of effective policies aimed at improving access and efficient administration of radiation therapy in an era of focusing on high-value care for patients.”