Arlene Sussman, MD, on COVID’s silver lining: Greater acceptance of telemammography
News on the public health crisis touched off by the spread of the novel coronavirus has been mostly bad. But a few bright rays have begun piercing the darkness. One is the growth of patient and provider acceptance of telemedicine. Significant swaths of the country have come to appreciate the tele option as a way to keep people safe without postponing appointments. These and other benefits afforded by the technology, so familiar to vRad’s clients, are now known to potentially millions more.
Meanwhile President Donald Trump recently issued an executive order for Medicare to expand telehealth coverage during the pandemic and make much of it permanent afterward.
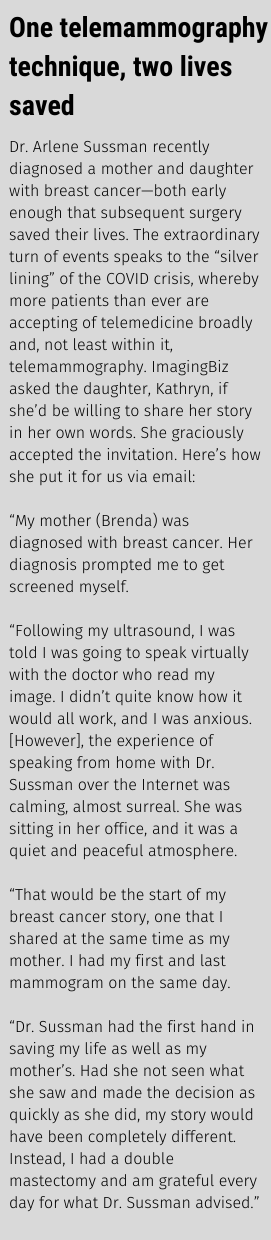
Given all this, telemammography seems on the cusp of bringing topnotch breast care to many women who otherwise may have gone without.
Arlene Sussman, MD, director of breast imaging for vRad, has seen COVID’s “silver lining” effect firsthand. She took our questions on life for patients and breast radiologists in a COVID-19 world.
When and how did you first get an inkling that the COVID crisis might open some doors for the field of telemammography?
It was when all outpatient services in radiology were pretty much closing. All hospitals were dedicating their time and resources to COVID patients. Things like mammography got back-burnered. Our volumes went to zero. We stopped the world for this virus, but cancer doesn’t know that. Cancer won’t wait.
I knew that we had a solution in place. It was just a matter of getting people to recognize that the value of telemammography was equal to—and in some way surpasses—the value of traditional mammography. As soon as everything started shutting down, we realized we didn’t have to shut down. We were already in place for people to access.
Do you expect tele to continue improving the state of breast care after the crisis subsides?
Oh yes. You think about this pandemic, and it just brings to light things that vRad has been hinting at for years. We’ve been thinking about opportunities to bring the benefits of telehealth to more people, and the pandemic has brought them to the forefront.
I mean, we [at vRad] have been doing telemedicine for quite awhile now. The pandemic just confirms in our minds what we always knew to be true. Which is that our telemammography program has great merit. So it’s great that so many [other providers] are getting on board with it. We’ve already worked through all the hiccups that they’ll be going through.
What are things like right now volume-wise?
Not only did we rebound back to normal, but our phones are ringing off the hook. In fact we’ve just signed some major contracts. For example, one of our large clients serves eight hospitals. They wanted to give all their patients virtual medicine opportunities. We had all eight of those hospitals up and running within 30 days of signing the contract. This reinforces telemammography as a service that’s well-received by everybody and whose time has really come.
We started our telemammography program few years ago. It’s as though COVID awakened people to the value of it.
What will keep the tele trend from fizzing out after COVID is under control?
A lot of people have come to see that tele is a true solution. Some people would argue that it’s become fashionable to do virtual medicine. But there’s more to it than just a marketing angle. Our telemammography team is a group of six subspecialists. It’s very hard to find another six-member group of subspecialized, fellowship-trained mammographers from around the country virtually sitting together, interconnected, offering a service like this to patients.
That will be hard to match by competitors of yours.
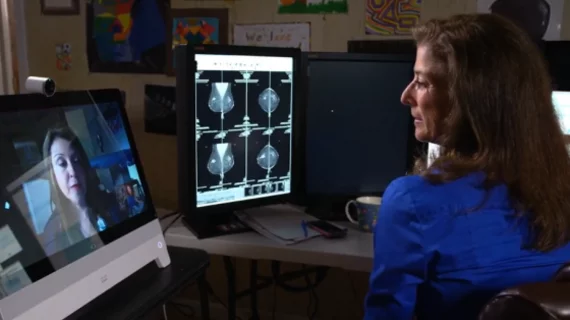
It will, and it’s only one thing that sets vRad apart. We’ve gotten very good at videostreaming with patients. Video can make a big difference when it’s done right. The patients and radiologist get a face-to-face encounter that’s perfectly safe from any risk of virus transmission. Everyone can keep their masks off, because clearly we’re social distancing.
Another thing that really makes it work for us is that there’s a whole body of regulation in this country directing how you must do telemammography or mammography in and of itself. There are FDA/MQSA rules and physicist qualifications and other mandatory details, and they vary by state. At vRad we have an administrative body that is 100% focused on compliance with all the varying sets of mandates across all 50 states. That’s all that group does.
That’s a great comfort to many of the mammography centers we work with. They don’t have to take those battles on. We do it for them. And it’s not like a chore we’d prefer to avoid—we embrace that part of our job. We actually enjoy it.
Can you envision telemammography emerging from the COVID crisis as a strong solution to the looming shortage of breast imaging specialists?
It is getting harder to find groups subspecialized in mammography, no question about that. There are a lot of complicated reasons why young radiologists don’t want to go into mammography in the numbers they once did.
One of the ways we’ve dealt with those kinds of challenges is by becoming very efficient in the cloud. Because the cases come to us, we can read so many more studies than if we were sitting in one room at one location. Our practice model for maximizing efficiency in mammography is really elegant in its simplicity.
What performance metrics do you have to show vRad’s clinical proficiency in the field?
Well, one that springs to mind is that, for 2D screening mammography, you should be calling back around 10% of your patients for additional imaging. For 3D tomosynthesis mammography, it should be around 5%.
Our team is well within the 5% to 10% range. We review that monthly, and we feed the metric back to all our team members. It’s not enough that some person who’s running the program is looking at the performance metrics on callbacks. The doctors themselves get that feedback every month. This tells them if they’re reading proficiently or not. So that’s a very important metric.
Does everyone see everyone else’s numbers or just their own?
All six team members see everything. Transparency on clinical performance is very important. We all want to provide superlative service. Seeing that metric every month keeps us in a constant state of professional skills improvement, both individually and as a team.
How and why did vRad build its own technology platform to optimize remote reading and personalized service?
In order to be optimized you have to be scalable. And all the software programs out there from equipment manufacturers and technology developers were very sluggish, just too slow for us. We were finding they couldn’t handle large volumes or deal with variations in mammography equipment from different manufacturers. The OEMs all have their own software or reading platform.
A doctor in the cloud can’t have eight different workstations based on what manufacturer’s machine was used to acquire the images. So we looked at those factors combined and decided to develop our own platform. We wanted it to be scalable and FDA-approved, of course, but it also had to let us read images acquired on any manufacturer’s mammography machine.
That’s what we developed and that’s what we have. It took over a year to develop and build. The engineers at vRad were quite dedicated. They did everything they needed to do to make sure it would pass all regulatory inspections. And they built in or have added some great bells and whistles—automated notation transmittals, stopping and zooming while viewing any give image, comparing new findings with priors.
We can now read any and every mammogram on our one universal platform. This has been invaluable to us.
How might telemammography emerge from the COVID crisis better than it’s ever been before?
Telemedicine really is taking off now and is here to stay. But every state has its own requirements for radiology. And the way the law is written right now is such that, in order to interpret a mammogram, you have to be licensed in the state in which the mammogram is performed. So I have to have 50—that’s five-o 50—state licenses.
Telemammography crosses state boundaries because it’s in the cloud. So why are we applying rules based on state boundaries to a national, cloud-based service? That’s what I would like to see changing post-COVID, as the silver lining in this dark cloud that is the COVID crisis.
What are you most looking forward to over the next few years?
I’d like to see vRad continue building our platform to make it as accessible as it can be regardless of the size of the facility, from the largest to the smallest. And I know that our people are working to make that happen. Everyone here is very forward-thinking. We’re always thinking about the next step—about how telehealth technologies might bring ease of access to more people who wouldn’t have access to a subspecialized radiologist.
I have personally reached out to women who otherwise wouldn’t have access to a breast subspecialist. These are women who deserve that kind of access, just like every woman who may live in some large metropolitan area. These are women who have to travel a couple of hours to get a mammogram. And now they have the opportunity to connect with me. For me it’s a great privilege to be able to help in a situation like that.
Learn More
Schedule a conversation with a vRad expert advisor to learn more about vRad’s Breast Imaging Service of Excellence.