The hidden costs of legacy image exchange solutions
Sponsored by PocketHealth
A survey of medical imaging leaders uncovers the hidden impacts of legacy image exchange solutions.
A recent 2024 PocketHealth survey of 202 U.S. hospital and imaging center decision-makers highlights the significant challenges healthcare providers face with legacy image exchange systems. The survey and conversations with industry leaders reveal that these outdated solutions impact both operational efficiency and patient satisfaction, often resulting in additional workload and increased costs. The survey identifies several ongoing issues, including:
In this article, we will share insights from the survey, summarize the limitations of legacy image exchange solutions and explain how a patient-centric approach can solve many of these challenges.
Looking to streamline workflows and create efficiencies? Download this white paper for more actionable insights.
Imaging centers
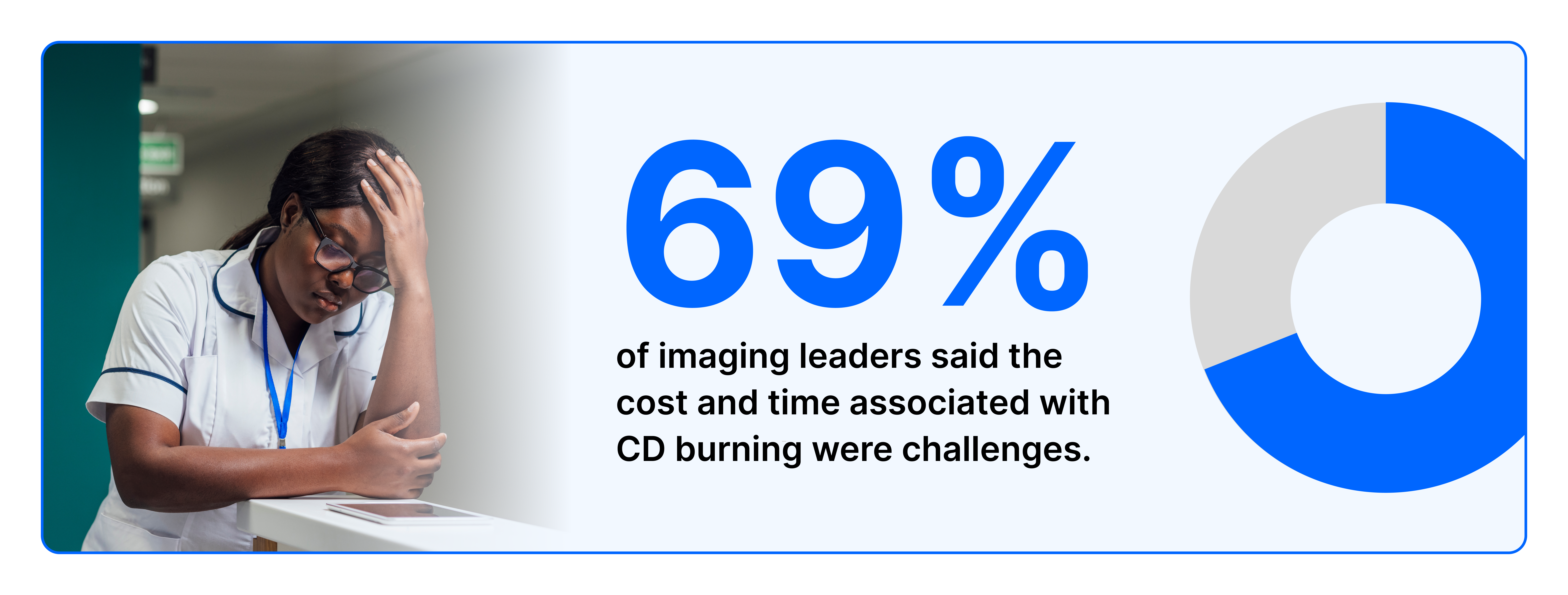
Due to network barriers, patients and referring physicians face difficulties accessing and sharing imaging which leads to reliance on CDs and manual workflows. A major concern for imaging centers is the substantial expenses related to burning CDs for patients, referring physicians, legal requests and out-of-network providers. In a 2024 PocketHealth survey of decision-makers in U.S. hospitals and imaging centers, 69% of respondents said the cost and time associated with CD burning were top-of-mind challenges. These expenses include the administrative overhead of buying, shipping, burning and distributing CDs—all processes which incur unnecessary costs for imaging centers.
Hospitals and health systems
Radiology management
Legacy systems require staff to manage multiple logins and navigate complex workflows across different platforms. Since staff resources are limited, these workflows take time away from high-value tasks. This complexity contributes to low adoption rates among patients and referring physicians and forces staff to rely on stop-gap solutions like CDs and VPNs. These complex workflows increase operational costs, create inefficiencies and negatively impact both patient and referring physician satisfaction.
IT departments
IT departments face challenges when integrating legacy systems with existing IT infrastructure. Managing multiple logins and workflows across various image exchange vendors can result in confusion, delays and inefficiencies. Another significant challenge involves maintaining data security and addressing privacy concerns—82% of IT leaders identify this as a challenge with their current image exchange solution.

Additionally, timely support from legacy vendors when addressing tickets is often lacking, leading to delays in resolving technical issues. These delays can slow down image sharing with patients and referring physicians and cause care delays.
Patient Experience
Legacy solutions often hinder patient engagement and empowerment, leading to lower patient satisfaction (HCAHPS) and Net Promoter Scores (NPS). Patients encounter difficulties accessing their records in diagnostic quality and receiving adequate education about their health—87% of imaging leaders highlight patient satisfaction as a challenge. Inconsistent communication practices and maintaining patient follow-up adherence are also ongoing struggles. These efforts are further compounded by staff burnout, resistance to change and inadequate training on patient engagement strategies

Health Information Management
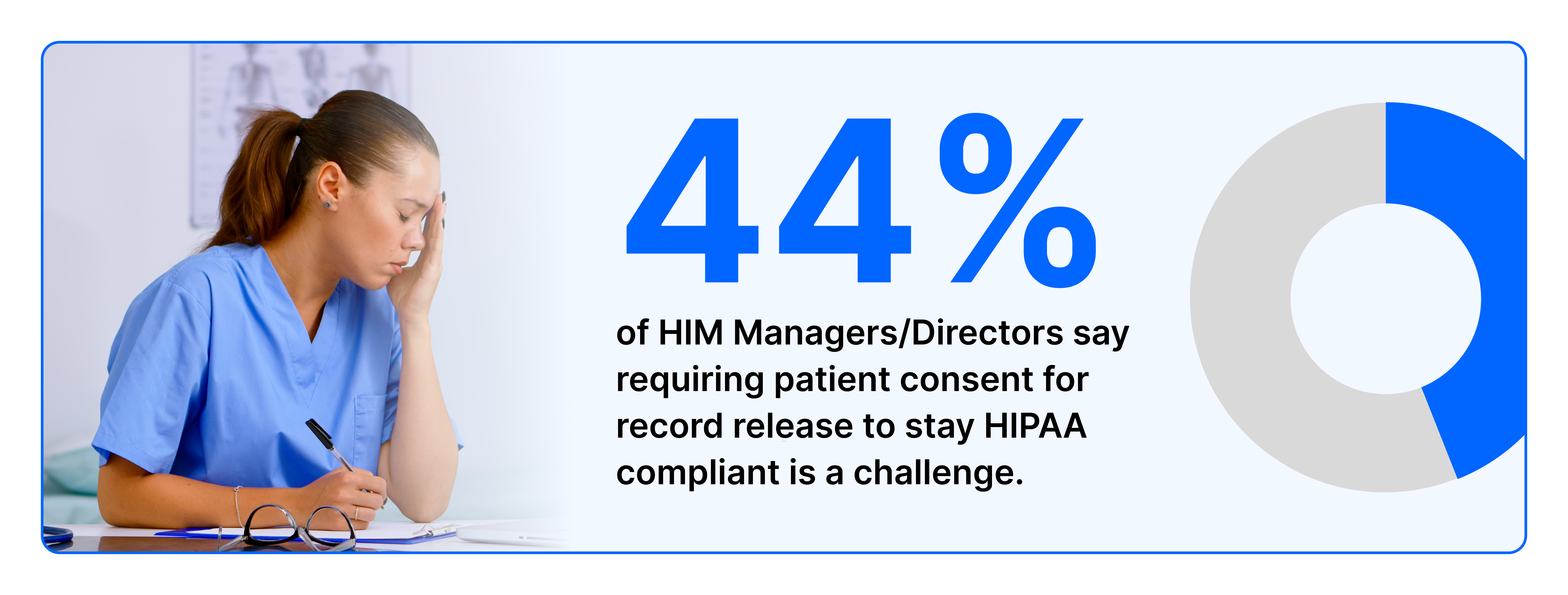
Fulfilling requests for patient data on time is a top priority for Health Information Management. Legacy solutions create care delays due to network barriers, which causes staff to rely on slower, more manual processes like burning CDs. Maintaining HIPAA compliance is also a key concern––44% of HIM Managers/Directors say requiring patient consent for record release to stay HIPAA compliant is a very relevant pain point. The risk of HIPAA violations—namely comprising patient privacy and security—increases when CDs containing sensitive patient data are lost or mishandled during urgent transfers.
Addressing the limitations of legacy solutions can be effectively achieved by introducing patient-centric solutions that streamline image exchange, enhance data security and improve overall patient engagement. Adopting patient-centricity offers a pathway for overcoming healthcare challenges and ensuring a more efficient and satisfying experience for patients, providers and referring physicians.
How PocketHealth solves healthcare challenges
PocketHealth modernizes image exchange through a patient-centric platform and solutions that prioritize accessibility, efficiency and patient experience. Unlike traditional legacy systems that have network restrictions and deemphasize patient access, PocketHealth streamlines image exchange. PocketHealth offers intelligent patient engagement functionality and tools that reduce costs and provide patients with quick and easy online access to their imaging records.
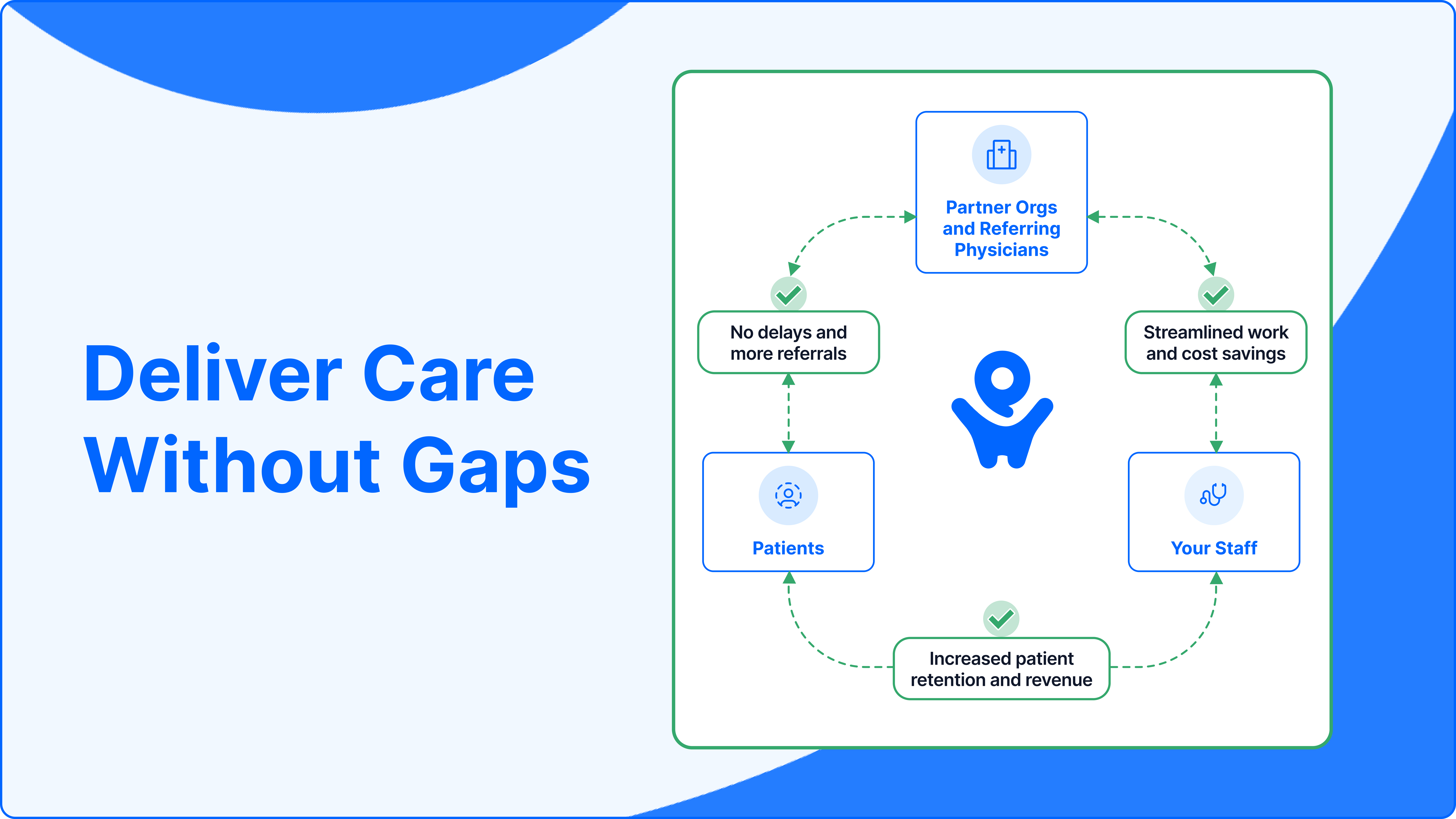
PocketHealth not only enhances patient understanding and involvement in their care but also simplifies workflows for providers, staff and referring physicians. PocketHealth's seamless, network-agnostic solution eliminates reliance on CDs by automating administrative tasks that typically consume staff time and energy. Unlike legacy image exchange systems, PocketHealth’s simple interface and efficient workflow ensure ease of use and fewer clicks for both patients and staff.
Learn how PocketHealth fills the gaps of legacy solutions and solves healthcare challenges.
