AI bests humans at predicting outcomes for brain radiotherapy patients
A new AI technique could be more successful at predicting radiotherapy outcomes for cancer patients with brain metastasis than the human eye, according to a study published in IEEE Journal of Translational Engineering in Health and Medicine [1].
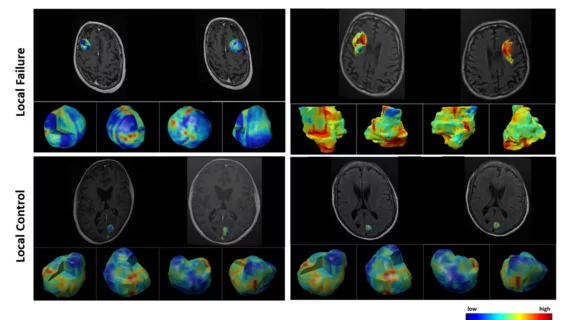
Researchers at York University in Toronto used AI neural networks trained via deep learning to assess 124 patients with brain metastasis based on their baseline MRI taken for treatment planning before radiotherapy. Two to three months after radiotherapy treatment, the patients underwent follow-up MRI and a radiation oncologist and neuroradiologist classified their lesions as Local Control—indicating a stable or shrinking tumor—or Local Failure—indicating an enlarging tumor.
The results revealed that certain characteristics of tumor or lesion margin areas in MRI images were important to predict radiotherapy treatment outcomes, with AI offering a way to assist humans in predicting treatment failure. While oncologists were able to predict treatment failure about 65% of the time, the best of several AI models was able to predict treatment failure with 83% accuracy.
“This is a sophisticated and comprehensive analysis of MRIs to find features and patterns that are not usually captured by the human eye,” Ali Sadeghi-Naini of York University’s Lassonde School of Engineering says in a news release.
Sadeghi-Naini also explained the critical nature of quickly assessing whether radiotherapy is effective for an individual patient.
“Not all of the tumors respond to radiation—up to 30% of these patients have continued growth of their tumor, even after treatment,” Sadeghi-Naini says. “This is often not discovered until months after treatment via follow-up MRI.”
Given that the median survival rate for brain metastasis patients after radiation therapy ranges from just 5 months to 4 years, as noted in the study, an early heads-up on potential treatment response can make a big difference.
“It’s very important to predict therapy response even before that therapy begins,” Sadeghi-Naini says.