What is the ROI on AI adoption in radiology?
Radiology by far has the largest penetration of artificial intelligence (AI) in medicine, but with minimal or no reimbursement, hospital administrators may ask where the return on investment (ROI) is to justify AI spending. Radiology Business spoke to several key opinion leaders to find out their thoughts on the value of AI.
The U.S. Food and Drug Administration (FDA) has now cleared well over 500 market-cleared AI medical algorithms as of January 2023. The vast majority of these are related to medical imaging. This includes 396 radiology algorithms. Cardiology has the second largest number of approvals at 58, many of which also are specific to cardiac imaging.
"We have seen from the U.S. FDA the number of cleared algorithms available for commercial use are escalating," explained Bibb Allen, MD, FACR, chief medical officer of the American College of Radiology (ACR) Data Science Institute and a past ACR president. But, he said, the adoption rate has been very slow. This is partly due to hospitals wanting assurances that the AI will work as intended and has clear evidence it will improve workflow, reduce costs and improve patient care. There also is a lack of reimbursement to cover the cost of adopting AI.
"I think finding the right AI tools and the right value proposition for the institutions is the main thing," Allen said. "On the payment and policy side, there are two reasonable arguments. As a radiologist, I believe it will provide us with safer and more effective care, whether that comes from decreases in turnaround times or decision support capabilities, or the identification of critical findings. On the other hand, the payer might say 'well wait a minute, we are already paying you, the radiologist and the expert, to make those same conclusions, so why should we on a fee for service basis provide additional payment?' And I think that is going to be a struggle for health policy makers."
Should AI gain reimbursement or is it just a practice expense?
The decision to adopt AI is not really up to the radiologist. Administrators or entire group practices must first figure out if AI adoption is worth the cost, explained Keith J. Dreyer, DO, PhD, chief science officer of the American College of Radiology (ACR) Data Science Institute. Often, that decision lies with hospital or health-system executives who do not understand the day-to-day work of a radiologist.
"There are not a lot of use cases today that have proven to a payer that AI is of value such that they are willing to reimburse the clinician who uses it. There is no reimbursement for PACS either, or for radiology information systems (RIS) or electronic health records (EHR), it's just a practice expense," Dreyer said. "So thinking of AI as a full category of its own, but just as a technology, then the question is does this technology make you more efficient? Does it bring is some new action that can improve care or make it faster so it is worth paying for it?"
Dreyer said the lack of reimbursement for AI might also dissuade health systems from spending more to purchase the technology. However, health systems need to consider if the technology can help enhance the workflow of radiologists to make them more efficient, or if AI could help improve patient outcomes.
"Is AI saving time for the radiologist such that you make them more efficient and it makes the AI worthy of purchasing?" Dreyer said. "I don't see any published evidence that would demonstrate that as 100% yes. I hear anecdotal stories and I have seen some small studies that have shown this, but I have not seen by and larger that this is the case. But, this will be on a case-by-case basis, because it is not just the use case as to the accuracy of the algorithm, it is also how it was implement that it can make you faster or slower."
AI may help address the growing shortage of radiologists
The role of AI is becoming more important as the U.S. faces a growing shortage of radiologists, explained Charles E. Kahn, Jr., MD MS, Editor of the the Radiological Society of North America (RSNA) journal Radiology: Artificial Intelligence, and professor and vice chair of radiology at the University of Pennsylvania Perelman School of Medicine. He said the technology can help augment radiologists to improve their workflow and make them more efficient. As an example, he said AI and do a first pass read to triage exams into suspected normal and suspected disease. This helps allow the radiologist to concentrate on reading cases with suspected disease or more complex cases.
This augmentation to help offset the shortage of radiologists was echoed by Ed Nicol, MD, consultant cardiologist, cardiac imager and honorary senior clinical lecturer with Kings College London. He is also president-elect of the Society of Cardiovascular Computed Tomography (SCCT). He said AI to do the simple but time consuming tasks and to help prioritize exams based on complexity is worth the cost to get more of what really matters from the human exam readers.
"We don't pay radiologists or cardiologists to draw lines around things, my 7 and 10 year olds can probably do as good a job on that. We also have AI systems that can do a first read and determine the first 10 cardiac CT scans are normal, and these 12 are abnormal. So you can get a cup of coffee and blast through the normals and then determine when you are fresh, or in the morning, go through the difficult ones. These technologies exist already, but we are not leveraging them. What we are really pay a radiologist or cardiologist for is to put the findings into context," Nicol explained.
What are the value propositions for radiology AI?
Allen outlined several key AI value propositions that hospitals should be considering.
"AI models can find things that radiologists cannot find, or we as radiologists just can't see," Allen said. This can includes figuring out a phenotype of a brain tumor using radiomics so the appropriate therapy can be chosen.
Population health is another area where AI can sift through vast amounts of imaging data to identify patients with key incidental findings for things like pulmonary embolism, coronary disease, pulmonary emphysema and hepatic steatosis.
"All of these things no one is going to care about when a patient is in the emergency department for diverticulitis. They are going to get antibiotics, and that is really the end of their episode of care," Allen described. "And the fact that they have hepatic steatosis, or they have coronary artery calcification, and they are only 40-years-old gets lost, even if we say it it just gets buried in the report or it does not make it to the problem list for follow-up. So this opportunistic AI screening for population health has a great chance for ROI."
For AI that can act as a second set of eyes for radiologists, that might be an area where the radiologists figure out what the value is on that type of algorithm for themselves. Even AI that can help detect cancers, lung nodules or other conditions in the non-acute setting may have benefits to prevent missing things in scans, or to act as a second opinion. As a second set of eyes for radiologists, AI can double check datasets to make sure nothing was overlooked, or to get a second opinion about a questionable area of an image. AI might also help detect rare conditions a radiologist might only come across a few times in their career.
"If we have that second set of eyes that helps us find more breast cancers, maybe that is valuable enough to us to give us that extra peace of mind," he said. Valuable enough to invest in the technology, even if there is no reimbursement.
But, opportunity for AI may also rest in conversion from a fee-for-service model to a value-based payment model.
"You can imagine in a value-based payment system, any tool that makes you more efficient, if you are getting paid the same, you can pay a little more for AI to become more efficient and it helps your bottom line," Allen explained.
AI that can automatically identify a pneumothorax on a mobile digital X-ray system, or alert clinical care teams of a suspected stroke, pulmonary embolism or other emergency conditions also could potentially improve patient outcomes.
Many AI algorithms also perform complex measurements that are reproducible, image reformatting, anatomical labeling, contouring anatomy, and other tasks that are time consuming. AI in these instances can help reduce the tedious manual processes and may help improve radiology report information and accuracy, while reducing the time it takes to read an exam, especially amid falling reimbursements to read exams.
The business case for AI to make radiology workflows more efficient
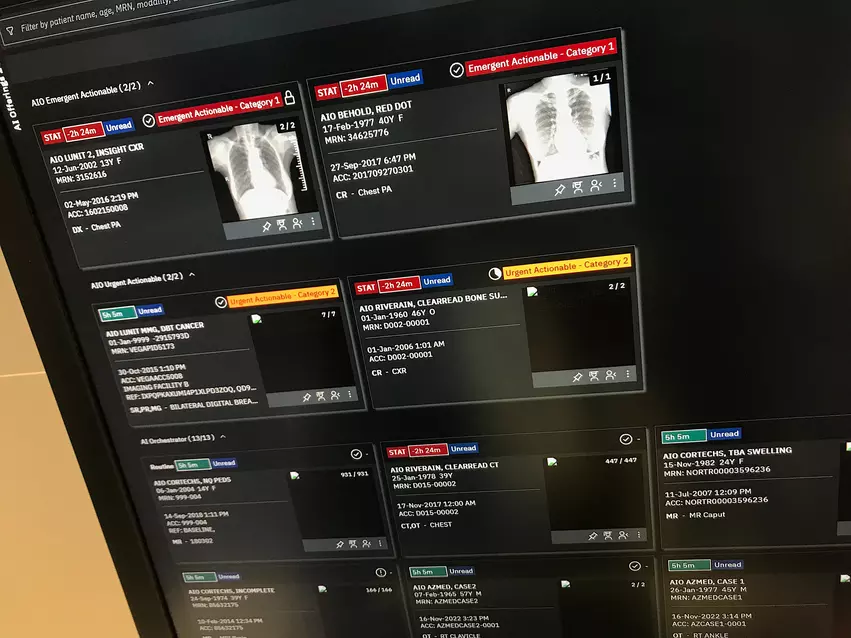
Anyone who has attended the large RSNA or Healthcare Information and Management Systems Society (HIMSS) meetings has seen PACS, enterprise imaging, workflow management and advanced visualization vendors adding complementary AI solutions that can enhance the radiology workflow. This includes AI for things like better organization of DICOM worklists in which critical findings may automatically move the exam to the top of the reading list, explained Sanjay Parekh, PhD, senior market analyst with Signify Research.
AI is also helping enable things like single-click marking of exams for follow-up for things like incident findings, automated measurements, automating things like anatomical countering and cardiac strain, or automatic ally calling up relevant priors for comparisons for tracking changes in tumors.
“It’s not just the image analysis, it’s also the workload balancing, the fleet management, or how do you get all these resources onto one platform to deliver value to the healthcare system, not just the radiologist,” Parekh said.
This includes looking at both upstream and downstream workflows and what clinicians need and how AI can be implemented to help facilitate better care by reducing bottlenecks or areas where there is a lot of manual data entry. In acute care this includes several AI vendors to aid acute care teams with alerts, immediate access to imaging and other patient data, and the ability to message everyone at the team before the images are even read by the radiologist.
How will AI change the future of radiology?
Parekh said there is a trend toward “opportunistic screening” by AI to search for incidental findings in all types of medical imaging that could help improve care by catching diseases before they become more advanced and symptomatic. This includes things like lung screening CT or virtual colonoscopy exams where AI algorithms look for calcium in the arteries to estimate cardiac risk scores, or scans the images for abnormal findings in the background unrelated to the purpose of the exam.
“This is looking downstream from radiology and saying, OK, we are picking something up opportunistically, but then we don’t want the patient to fall off the radar. You want that to be followed up,” Parekh says.
Opportunistic screening may offer ways for hospitals to better care for patients preemptively rather than being reactive to acute episodes or long after a cancer had become a serious problem and is more difficult to treat.
Allen said AI that can help facilitate that followup process also could be worth the expense if it brings in additional business for the healthcare system.
Parekh said the American Medical Association (AMA) now has CPT codes to track usage of AI technology, which is a first step when evaluating if new technologies should receive reimbursement.
Even if AI is not reimbursed, Parekh said healthcare providers need to look at whether AI can help improve patient outcomes and save money in other areas, which could make the investment in AI worthwhile. Beyond opportunistic screening, if AI apps can help save radiologists enough time to be able to read a few more exams each day, there could be business ROI over the long term.
AI may help address health disparities
"We have not seen good payment models, so one of the fears that we have is that larger academic research centers will be able to adopt AI into clinical use, while smaller practices, particularly in underserved areas, are going to struggle without a reimbursement plan and create health disparities that I don't think anyone wants to see," Allen explained.
Kahn also said AI may play a key role in the coming years of addressing health disparities.
"At some level, we need to find ways to where we can deliver care that is cost-effective, reaches all the people we need to reach and provided equitable healthcare, and the hope is that we can use AI to expand the reach of what we o and improve the quality of it," Kahn said.
Allen agreed AI can help close areas of health disparities, which is of interest for health system administrators and possibly to payers.