Biopsy before ablation has no cost advantage over both-at-once approach
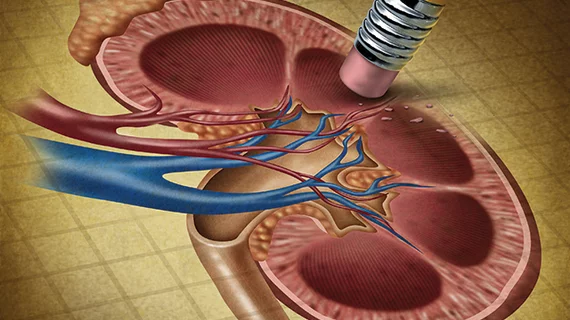
Established guidelines recommend biopsying small tumors of the kidney ahead of any procedure to ablate them.
A new study shows doing both at the same time can be a clinically sound and cost-effective alternative.
The study was conducted at Western University in Ontario and published May 15 in the Journal of Vascular and Interventional Radiology.
For the research, corresponding author Alexandru Florea, MD, and colleagues developed a decision-analytic model based on a cohort of 65-year-old men who had been treated for small, incidentally discovered renal masses of 1 to 3 centimeters.
The team used a decision tree to model the patients’ first year of clinical intervention. For subsequent years they used a Markov Model with a lifetime horizon.
The researchers assumed all patients to have been treated consistent with clinical practice guidelines as published by various medical groups.
Florea and co-authors note that all major urology and interventional radiology groups in North America and Europe recommend biopsy upon discovery of renal lesions, but groups differ on whether the biopsy is best performed ahead of the ablation procedure or during it.
For example, the American Urology Association and European Association of Urology call for biopsy prior to ablation.
On the other hand, the Society of Interventional Radiology maintains that either approach is acceptable and appropriate.
Simultaneous has the edge on QALY cost-effectiveness
Assuming members of the cohort were treated consistently with the guidance regarding surveillance, repeat ablation for recurrence, and systemic therapy for metastasis, Florea and team determined healthcare cost and utility values from published literature or local hospital estimates.
They calculated total lifetime costs from the perspective of a Canadian healthcare payer in 2022 Canadian dollars.
Key among their findings: The incremental cost effectiveness ratio (ICER) for simultaneous biopsy and ablation was found to be $8,494 per quality-adjusted life-year (QALY) gained.
Further, the biopsy-first approach was only cost effective when life-years were not quality-adjusted, and ablation cost was greater than $4,300 or benign mass prevalence was greater than 28%.
“The results of this study suggest that concurrent biopsy and ablation is a cost-effective strategy relative to sequential biopsy and ablation in the management of incidental small renal mass being considered for ablation,” Florea et al. conclude.
Uncertain dollar-to-dollar comparisons
The authors acknowledge limitations in their study design. Among these is the questionable generalizability of cost data from a single academic hospital.
“Institutional differences, including equipment and professional fees, as well as protocol variances such as length of stay within to recovery unit, or utilization of CT image guidance,” they add, “can lead to higher ablation procedural costs and may reach the threshold that would make pre-treatment biopsy cost-effective.”
In addition, they note, the analysis was conducted from the perspective of a Canadian healthcare payer. Given this starting point, results “may apply to the U.S. context to the extent that the Canadian fee structures are similar to the Medicare fee structures.”
There’s more, and the journal has posted the study in full for free.