Expedited g-tube placement cuts costs and LOS in head and neck cancer patients
Use of a multidisciplinary team (MDT) for the implementation of an expedited, image-guided outpatient gastrostomy tube (g-tube) placement pathway for head and neck cancer patients (HNC) decreased procedure costs by $2,940 and reduced hospital stays, according to a new study in Academic Radiology.[1]
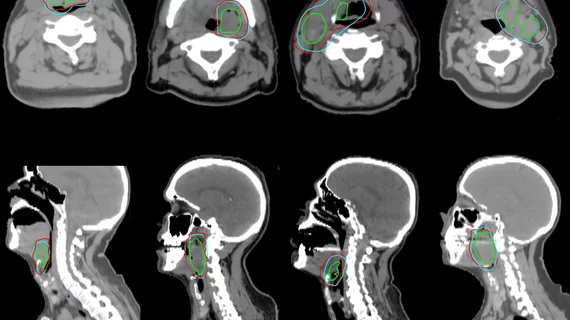
Researchers at the UC San Diego, La Jolla, California, performed a retrospective study of 142 patients who underwent elective image-guided g-tube placement performed by interventional radiology between 2015-2022. These patients were divided with 52 having undergone the traditional pathway, and 90 patients using an expedited pathway. The goal was to compare whether the use of an expedited g-tube placement MDT, consisting of interventional radiology, oncology, surgery, nutrition and speech language pathology departments, led to improved outcomes.
"This single center experience with consolidating the clinical decision-making process in an MDT and improving patient access to nutrition education mitigated hurdles to and decreased costs associated with image guided g-tube placement in HNC patients. Such a protocol was found to be equally safe with no statistical difference in overall complication rates between the traditional and expedited groups," the researchers explained in the study.
Use of an MDT successfully provided enteral nutrition support faster, with lower associated costs. The researchers said the 90-day complication rate was comparable between groups. The expedited pathway decreased the time from consult to procedure by 11.1 days and decreased charges per procedure.
The placement of g-tubes in HNC patients undergoing multi-modal therapy is important because they often have debilitating treatment-related adverse events, including dysphagia, mucositis and anorexia. G-tube placement protocols are not standardized across different hospital systems so researchers said this study was an attempt to look at two different approaches used at UC San Diego.
This study was partially supported by a National Institutes of Health grant.