The CCTA Playbook: A Guide to Coding, Reimbursement and Operations
(2022 updated content at the bottom of the page)
A compendium of the business intelligence required to launch a coronary CT angiography (CCTA) service In the United States, unspecified chest pain is the second most common reason for an emergency-department visit. Each year, 5 million to 8 million patients present to the emergency department with chest pain. In 2004 alone, more than 6 million patients presented to U.S. emergency departments with acute chest pain. Of these patients, 4% to 5% have a coronary event that is not properly diagnosed, resulting in an erroneous discharge from the emergency department.
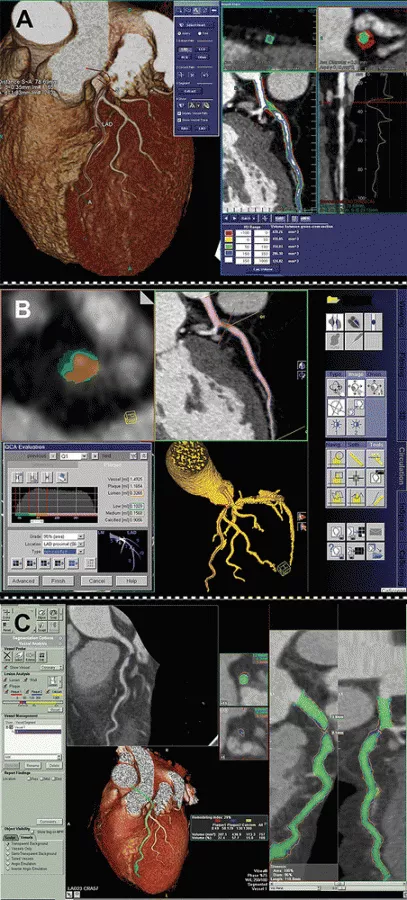
Approximately 40% of elective stress tests will yield false-positive results, but only about 13% of CCTA exams (see Figures 1 through 4) will have potentially false-positive results. The lower false-positive rate should mean better patient care and cost savings, which should be important to payors.
Market forces for coronary CT angiography
In an acute situation, CCTA could result in cost savings and better patient care by decreasing unnecessary hospital admissions for chest pain. In addition, its use could decrease the incidence of patients being discharged from the hospital if they have true disease. In a 2007 study,[1] 54 low-risk patients with chest pain who showed no acute ischemia on ECG then underwent CCTA. None of the 46 (85%) patients who were discharged following negative CCTA results experienced any coronary complications within the 30-day follow-up period.
These findings support the conclusion that CCTA may safely allow rapid discharge of patients with negative studies. Given the well-documented sensitivity and specificity of CCTA, why is there hesitation to reimburse for this exam on a uniform national level? For a potentially heavily utilized study, payors want outcomes data before approving reimbursement for new technologies.
In the case of imaging, that information can be extremely difficult to obtain. Drugs and medical devices may have measurable effects on patient outcomes, but diagnostic technologies have a less direct connection with patient outcomes because outcomes are more likely to be altered by treatment decisions and patient compliance, among other nonimaging factors. It is clear, however, that utilization of radiology services is increasing.
Diagnostic imaging services paid for under Medicare’s physician fee schedule grew more rapidly than any other type of physician service between 1999 and 2003. During the same period, the average growth in physician services was 22%, but for imaging, it was 45%. Imaging costs are growing at twice the rate of prescription-drug costs, and may continue to grow at an accelerated rate. These figures make imaging a target for cost cutting, even in areas where imaging has great potential to reduce the total cost of care.
In 2007, for example, CMS proposed a restrictive national coverage determination that would have required coverage with evidence development, effectively restricting CCTA to research settings. In January 2008, six professional societies informed CMS that, if implemented, this policy would have a profoundly negative effect on Medicare beneficiaries by limiting needed access to CCTA for clinically appropriate indications. In response to this and other public commentary, CMS withdrew its proposal in March 2008, allowing Medicare carriers to retain their own local coverage determinations.
Until payors become convinced by further research that coronary CT angiography replaces other tests (instead of being added to them), a national coverage decision resulting in the creation of category-I CPT codes for CCTA is unlikely to be made.
Coding for cardiac CT exams
There are eight current CPT codes in category III that are applicable to CCTA. They include:
• 0144T — for CT of the heart without contrast material, including image post-processing and quantitative evaluation of coronary calcium.
• 0145T, for cardiac structure and morphology, CT of the heart before and after contrast administration and further sections, including cardiac gating and 3D image post-processing.
• 0146T, for CTA of the coronary arteries (including native and anomalous coronaries and bypass grafts) without evaluation of calcium.
• 0147T, for CTA of the coronary arteries with evaluation of coronary-artery calcium.
• 0148T, for cardiac structure and morphology with CTA of the coronaries and without coronary calcium scoring.
• 0149T, for cardiac structure and morphology with CTA of the coronaries with coronary calcium scoring.
• 0150T, for cardiac structure and morphology in congenital heart disease.
• +0151T, an add-on code for function evaluation (left and right ventricular function, ejection fraction, and segmental wall motion).
In general, codes that specify structure and morphology are for use with pre-electrophysiology CT studies. These may be ablations, in which the atria and pulmonary veins are being evaluated by CT, or may be evaluations of the cardiac venous system in anticipation of biventricular pacemaker placement. There are, at present, two separate category-I codes for 3D rendering, but they should not be used for CCTA because 3D imaging is already included in the T codes.
The triple–rule-out CCTA study is often ordered to evaluate the patient for coronary-artery stenosis, aortic dissection, and pulmonary embolism. For this study, it is possible to use two codes: 71275 (conventional CTA evaluation of the aorta and pulmonary vessels) and 0146T (CTA of the coronary arteries).
Billing for both codes might require advance beneficiary notice for the T code plus a modifier of reduced professional service for one of the codes (a 52 modifier); this may be difficult if the patient is in acute distress. For this reason, it may be preferable to bill for the category-I code (71275) and write off the cardiac portion of the exam.
ICD-9 codes supporting medical necessity for 0146T and 0147T (CTA) are 413.0, 413.1, and 413.9 (angina pectoris, decubitus, Prinzmetal, and unspecified angina); 427.31 and 427.32 (atrial fibrillation/flutter); 786.50, 786.51, and 786.59 (chest pain: unspecified, precordial, and other chest pain); 747.41 and 747.42 (total/partial anomalous pulmonary venous return); 786.05 (shortness of breath); 414.8, 425.4, and 746.85 (chronic ischemic heart disease, cardiomyopathy, and congenital heart anomalies); 428.0 (congestive heart failure, unspecified); and 794.30 (cardiovascular, abnormal function study, unspecified). ICD-9 codes supporting medical necessity for cardiac structure and morphology codes 0145T, 0148T, and 0149T include 427.31/427.32 (atrial fibrillation/atrial flutter); 428.0 (congestive heart failure, unspecified); and 425.4 (other primary cardiomyopathies).
View the CMS website for the newest information on CCTA CPT code.
Reimbursement for CCTA
At this time, and in all cases, the professional component for CCTA reimbursement is carrier priced (locally determined). When CCTA is performed in an outpatient imaging center, the technical component is carrier priced. Each carrier issues its own policy (local coverage determination) regarding category-III codes. These determinations state whether the code will be reimbursable and what criteria must be met for reimbursement.
All 50 states have local coverage determinations in place for CCTA, and many are based on common language taken from a model originally submitted by the ACR and other professional societies. In one example of a carrier’s local coverage determination on CCTA reimbursement, Wisconsin Physician Services (the local Medicare carrier for Wisconsin, Illinois, Michigan, and Minnesota) specifies the four main categories of indications for which CCTA will be reimbursable.
The first category is CCTA used as an alternative to invasive angiography following an equivocal stress test or one that is suspected to be inaccurate. CCTA, in this case, could provide a separate method of assessing coronary arteries (different from a stress test) and limit the number of normal invasive coronary angiograms. CCTA may also help clinicians avoid missing coronary-artery disease in patients suspected of having undergone inaccurate stress tests.
The second indication category is evaluation of acute pain in the emergency department. The exam can be used to triage patients quickly in the emergency department and limit resource use in chest-pain patients who do not have coronary-artery disease.
The third category is assessment of coronary or pulmonary venous anatomy. This includes presurgical planning prior to pacemaker placement or pulmonary vein catheter ablation to eliminate recurrent atrial fibrillation. The fourth category is assessment of suspected congenital anomalies of coronary circulation. Here, CCTA allows further characterization of the presence of (and possible harm from) congenital abnormalities; it may also be useful for surgical planning in such cases.
Wisconsin Physician Services also imposes six exclusion criteria that may be typical of those found elsewhere.
First, the test is never covered for screening in asymptomatic patients.
Second, the test may be denied on postpayment review if there is sufficient pretest knowledge of extensive calcification of the coronary segment that would diminish interpretive value.
Third, the multidetector CT used must have at least 64 slices per rotation and high-resolution slices of 1 mm or less.
Fourth, all studies must be ordered by a physician or a qualified nonphysician practitioner. Fifth, when contrast is given, a physician must be present for direct supervision during testing.
Sixth, atrial fibrillation, by itself, is not an indication, but atrial fibrillation with planned ablation is allowed.
It should be noted that CCTA codes include the administration of beta blockers and the monitoring of the patient during the exam by a physician who is experienced in the use of cardiovascular drugs, so these are not separately payable services. Likewise, the administration of sublingual nitroglycerin is unlikely to be separately payable, although it may improve results by dilating the coronary arteries before scanning.
Cardiac CT post-processing software can help define the details of soft plaque, calcium, stents, blockages and anatomy. With the addition of FFR-CT, physiological information can also be gained from the noninvasive imaging. This can help determine if a patient can be treated medically or if they need to be revascularized using a stent.
Medicare coverage for repeat CCTA examinations is also determined by individual carriers, but reimbursement for frequent CCTA repetition is probably unlikely. The frequency of the studies must be reasonable and justified by the course of the patient’s illness, according to some carriers’ utilization guidelines; this means that reimbursement may be denied for repeat tests for the same patient.
In California, one Medicare carrier, National Heritage Insurance Co, has stated that it is not normally reasonable to repeat CCTA in less than five years if the patient’s calcium score is less than 10 (or the equivalent) on the initial study; when the score is higher than 10, it is not usually necessary to repeat the study in less than three years.
Empire Medicare, a carrier for New York and New Jersey, stresses the need for CCTA to produce usable information. It states that the selection of the test should be made within the context of other testing modalities, such as stress myocardial perfusion images or cardiac ultrasound results, so that the resulting information facilitates the management decision instead of merely adding a new layer of testing.
Planning for CCTA reimbursement
Because of variations in local carriers’ policies and general uncertainty, it is difficult to predict the reimbursement level that CCTA will eventually reach. Local carriers and private insurers do reimburse for CCTA, but it is important to ask at what payment rate they do so. Some carriers have published the applicable rates, but these can not be used to predict the eventual category-I reimbursement level. Accurate prediction is not possible because the data now being collected by the AMA on the utilization frequency of the eight category-III codes will influence which of these codes will survive the migration to category I, as well as whether some of the codes will be eliminated or augmented.
It seems safe to predict, however, that total Medicare payments for CCTA will continue to rise.
In 2006, Medicare paid for roughly 70,000 CCTA exams at a cost of $40 million to $50 million. As more facilities perform CCTA, this amount will increase. To limit overall expenditures, local rates could change (perhaps negatively) over time. If it isn’t possible to predict rates, how can providers approach planning for CCTA provision? Today, the best approach is to examine the nonfinancial factors carefully, in addition to speaking to carriers individually about their policies concerning the CCTA codes. Use of the self-pay system may also be feasible for patients who are not eligible for third-party reimbursement.
Additional Reading - CCTA Standards and Turf CCTA Staffing and Coverage
About the Author: Jonathan Berlin, MD, MBA, FACR, is a clinical professor of radiology at NorthShore University HealthSystem in the Chicago area. He has a master of business administration (MBA) degree in health/healthcare administration and management.
Updated Cardiac CT Content as of 2022:
VIDEO: The role of cardiac CT in the 2021 chest pain guidelines — Interview with Ron Blankstein, MD
VIDEO: Office-based cardiac CT and FFR-CT offer a new business model
Cardiac CT soft plaque assessment my offer paradigm shift for coronary disease screening
VIDEO: The new role of cardiac CT under the 2021 chest pain evaluation guidelines — Interview with Eric Williamson, MD
VIDEO: Cardiac CT now recommended as a front-line chest pain assessment tool — Interview with Leslee Shaw, PhD
VIDEO: The new role of cardiac CT in chest pain evaluation — Interview with Brian Ghoshhajra, MD
PHOTO GALLERY: Cardiac CT advances at SCCT 2022
VIDEO: Cardiac CT now recommended as a front-line chest pain assessment tool — Interview with Leslee Shaw, PhD
PHOTO GALLERY: Duly Health adopts outpatient cardiac CT as a standard of care
VIDEO: Use of CT to assess coronary plaques — Interview with Leslee Shaw, PhD
Expert panel recommends coronary CTA as first choice when evaluating for stable CAD
VIDEO: Cardiac CT training requirements for radiologists and technologists
New CAD-RADS 2.0 reporting for coronary CTA offers patient management recommendations
Find more cardiac CT news and video
Reference: