HHS chief defends controversial surprise billing provision, urging docs to ‘tighten their belt’
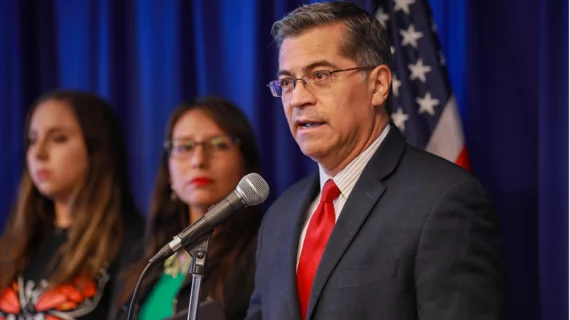
Health and Human Services Secretary Xavier Becerra is defending a key provision in a recently released rule to address surprise medical bills, which is opposed by radiologists and other physicians.
The federal government is proposing to ban the practice of issuing unexpected IOUs for out-of-network care. Physicians have said they support the effort. But they’re concerned HHS and other agencies are ignoring Congressional and favoring insurers by making the “qualifying payment amount” the crux of such payer-provider negotiations.
Becerra defended the final rule Monday, emphasizing HHS’ intent is to protect patients and drive down prices.
“I don’t think when someone is overcharging, that it’s going to hurt the overcharger to now have to [accept] a fair price,” he told Kaiser Health News. “Those who are overcharging either have to tighten their belt and do it better, or they don’t last in the business.”
The American College of Radiology and numerous other doc groups have advocated for using several factors to settle disputes, beyond the QPA (generally, the median contracted rate for services in a geographic area). Quality of outcomes, market share, complexity of services, case mix, and prior contract history are a few suggestions. More than 150 members of Congress are pressuring the administration to adopt this approach, alongside tens of thousands of physicians.
But Becerra is concerned broadening the process too much could increase costs. He highlighted a recent HHS report, which found that states using an approach similar to what physicians are recommending have seen healthcare costs rise.
“When the arbitration process is wide open, no boundaries, at the end of the day healthcare costs go up, not down,” Becerra told the news site. “We want costs to go down. And so, we want to set up a system that helps provide the guideposts to keep us efficient, transparent and cost-effective.”
The interim rule is slated to go into effect on Jan. 1. Rules this far along in the process are rarely changed, Kaiser Health News reported, but Becerra said HHS will continue listening. Read more from the interview below.