Amid lawsuits, radiologist opposition, Biden administration touts start of surprise medical bill ban
Amid multiple lawsuits and opposition from radiologists and other physicians, the Biden administration touted the start of its new ban of surprise medical bills on Monday.
The No Surprises Act went into effect Jan. 1, shielding privately insured consumers from receiving unexpected IOUs for out-of-network care in most instances. In addition, the law will require that providers give uninsured and self-pay patients overviews of their expected costs, among other key information, Health and Human Services said in an announcement.
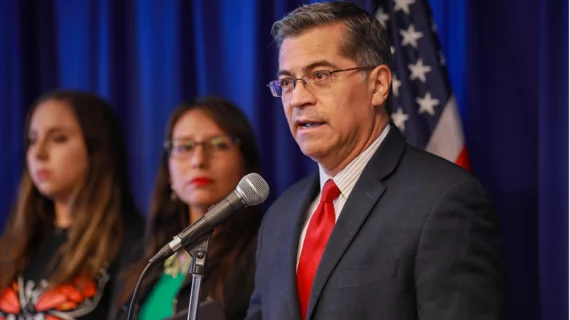
HHS Secretary Xavier Becerra believes these changes mark the “most critical consumer protection law” since the Affordable Care Act of 2010.
“After years of bipartisan effort, we are finally providing hardworking Americans with the federal guardrails needed to shield them from surprise medical bills,” he said in a Jan. 3 statement. “We are taking patients out of the middle of the food fight between insurers and providers and ensuring they aren’t met with eye-popping, bankruptcy-inducing medical bills.”
Becerra pointed to a recent HHS report, which found that nearly 1 in 5 privately insured patients receive a surprise bill after elective surgery, visiting an ED or giving birth. On average, the cost could range from $750 to upward of $2,600, according to the HHS Office of the Assistant Secretary for Planning and Evaluation.
Along with banning unanticipated bills, the No Surprises Act requires that cost sharing for emergency services is based on the in-network rate, regardless of prior authorization. It would also forbid bills from certain out-of-network providers when patients visit an in-network hospital for a procedure. And facilities must now share easy-to-understand notices, detailing such new protections and who patients can contact if they believe providers are violating the new law, HHS said.
“For services provided in 2022, you can dispute a medical bill if your final charges are at least $400 higher than your good faith estimate and you file your dispute claim within 120 days of the date on your bill,” the administration said in a corresponding fact sheet.
The announcement comes after several provider groups including the American College of Radiology filed suit to stop one key provision in the No Surprises Act. ACR and others have said they support efforts to protect patients from financial harm. However, they’re concerned the newly established process to settle payer-provider reimbursement disputes is skewed in favor of commercial insurers.