Radiation oncology relatively low in ‘hazardous attitudes,’ although ‘macho’ makes the radar
The Federal Aviation Administration assesses pilots for five “hazardous attitudes” that may forewarn of risky behaviors in the air. Therapeutic radiology researchers have adapted the FAA scale for radiation oncologists making treatment decisions.
Asking email survey recipients to react to declarative statements and hypothetical treatment scenarios, the team found low levels of hazardous attitudes in ROs as compared with not only pilots but also surgeons.
However, a hazardous attitude nicknamed “macho”—the signature saying of which is “I can do it”—attached to some 15.6% of the field.
Tellingly, this attitude correlated with nonadherence to Choosing Wisely recommendations.
Yet, despite the nickname, the macho hazardous attitude was not significantly associated with men, as “gender was not significantly associated with hazardous levels of any attitude,” report the authors, who were led by Nadia Saeed, BA, and Adriana Blakaj, MD, PhD, both of Yale. Senior study author was Suzanne Evans, MD, MPH, also of Yale.
Advances in Radiation Oncology, the scientific journal of the American Society for Radiation Oncology (ASTRO), presents the study in its November edition [1].
Predicting Who Will, Won’t Stick with Choosing Wisely
Saeed and co-researchers sent their survey to 809 radiation oncologists working in or near the country’s top 25 cancer centers.
Of 139 completed and returned surveys, 103 met the project’s eligibility criteria. Respondent ages were evenly distributed, 40% of the field was female, and 83% worked in academic settings.
The agree/disagree statements in the survey, 30 in number, were along the lines of “I like to practice unusual treatment paradigms in radiation oncology.”
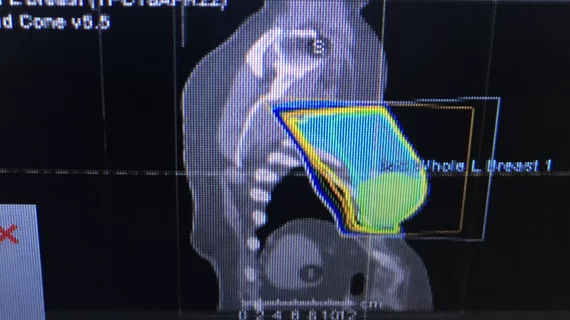
The treatment scenarios followed with queries about treatment preferences—for example, “radiation therapy allocation for an elderly woman with stage I breast cancer eligible for RT omission.”
The survey’s wording reflected ASTRO recommendations, and responses were classified as compliant or noncompliant with Choosing Wisely guidelines.
The five hazardous attitudes in the FAA’s scale and adapted for the radiation oncology survey:
- Antiauthority. Defining statement: “Don’t tell me.” (Antidote attitude: Follow the rules. They are usually right.)
- Resignation. Defining statement: “What’s the use?” (Antidote attitude: I’m not helpless. I can make a difference.)
- Impulsivity. Defining statement: “Do it quickly.” (Antidote attitude: Not so fast. Think first.)
- Invulnerability. Defining statement: “It won’t happen to me.” (Antidote attitude: It could happen to me.)
- Macho. Defining statement: “I can do it.” (Antidote attitude: Taking chances is foolish.)
Analyzing responses, the team found median scores for all five hazardous attitudes fell below those for pilots and surgeons.
Also, radiation oncologists older than 50 and with more than five years of experience were 4.45 times more inclined to prescribe or recommend risk-tolerant treatments for organs at risk than younger and lesser-experienced peers.
Further, physicians who credited careful planning for avoiding a complication in the past were almost five times more likely to recommend retreatment, even for higher-risk patients.
More Years of Experience = More Likely to Prioritize Suppressing Cancer Recurrence (over Avoiding Treatment Complications)?
In their discussion the authors speculate the increased willingness of older, more experienced physicians to abide risk-tolerant radiotherapy prescriptions may reflect “the influence of the 3-dimensional era, in which more dose-volume metrics are available, shifting focus to preventing complications.”
Another possible explanation they offer is a shift, made over time, away from avoiding treatment complications and toward suppressing cancer recurrence.
The authors acknowledge several limitations in their study design. Among these are potential nonresponse bias, overweighted ratio of academic radiation oncologists.
More:
The influence of training site, disease-site specialization, local practice culture, peer influence, and era of training cannot be reliably assessed by these data but is likely to contribute to prescribing preferences. In addition, given that prescribing too much or too little radiation therapy can both be risky, it would be worthwhile to determine whether hazardous attitudes are correlated with prescriptions that are risk tolerant for recurrence.”
The authors believe theirs is the first study examining physician attitudes in the field of radiation oncology, and they state that the work “lays the foundation for further efforts to identify factors associated with physician decision-making in this field.”
The study is available in full for free.