Clinical exams alone don’t cut it for breast cancer screening in women under 40
Despite low prevalence in the demographic, women younger than 40 years old should still undergo triple assessment for breast cancer—especially if they present with a symptomatic lump or have extensive family history, a team of U.K. researchers reported in Clinical Radiology this month.
Climbing rates of breast cancer in women across the world has prompted a global push toward early detection, prevention and treatment of the disease, first author Fayyaz Ali Khan Mazari, MS, PhD, and colleagues said, but the renewed effort to spread awareness has also led to more screening referrals than radiology facilities can handle.
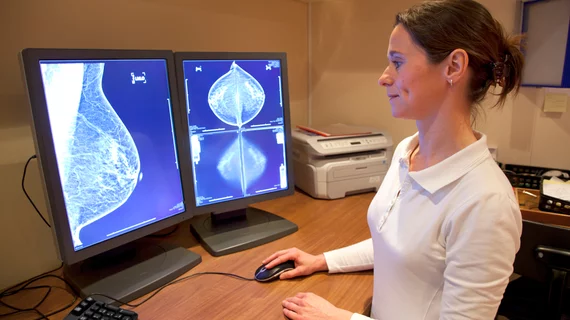
“All new referrals undergo triple assessment with clinical examination, radiological imaging and biopsy in accordance with the best practice guidelines and National Institute of Health and Care Excellence quality standard,” the authors wrote. “As all new referrals to breast care units have to be seen within two weeks, in accordance with National Health Service targets, this generates a considerable pressure on the resources of breast units, as one-stop clinically allied immediate radiology slots are limited.”
In the U.K., Mazari et al. said, the issue has raised the question of whether full triple assessment is necessary in such a young population, and whether it would be more efficient to omit imaging altogether in the age group. Because final diagnosis is unknown at the time of an initial visit, the authors wrote, each patient—regardless of age, history or risk—receives the same time allocation for appointments. Younger women, whose symptoms are likely benign, may take time away from older patients with a high-risk history of breast cancer and possibly malignant tumors.
“The vast majority of patients referred to the one-stop breast clinic under the current referral guidelines are young, with a low-risk family history and benign clinical examination,” the team wrote.
The researchers retrospectively collected data for all women under 40 who were seen at their one-stop Leeds Breast Unit between January 2014 and August 2015, noting demographics, symptoms, diagnostics and treatment details. Of the 3,305 patients ultimately included in the study, Mazaria and co-authors said, 95.6 percent were first-time referrals, 57.6 percent presented with a breast lump and 4 percent had a high-risk family history.
Breast cancer was eventually diagnosed in less than 1 percent of cases, according to the study—but for Mazaria and his team, that was enough.
“The results confirmed that the incidence of breast cancer remained very low in this cohort,” they said. “[But] this cohort should not be treated any differently regarding one-stop clinic infrastructure ... missing a cancer in this age group is a personal tragedy for the patient and her family, and can lead to significant medicolegal implications for the clinicians and healthcare providers.”
In line with NHS standards, the authors said average referral-to-diagnosis time was 13 days, while referral-to-surgery time topped out around 44 days. Three-quarters of the study population underwent imaging, 16.7 percent opted for a biopsy and 3.2 percent had surgery. All patients who were diagnosed with cancer were first-time referrals whose cancers were identified as suspicious lumps upon clinical examination and were diagnosed upon imaging.
Older age, as well as the presence of a breast lump, remained the two most key risk factors for diagnosis, Mazari and colleagues reported.
“Patients younger than 40 years who present with breast-related symptoms should be assessed with standard complete triple assessment, including radiological imaging,” they wrote. “Omission of radiological imaging in these patients can lead to missing a cancer diagnosis, as clinical examination alone cannot conclusively rule out malignancy.”