Nearly 40% of thyroid ultrasounds at 1 hospital had no noteworthy clinical findings
Nearly 40% of thyroid ultrasounds at one hospital had no noteworthy clinical findings, according to new research.
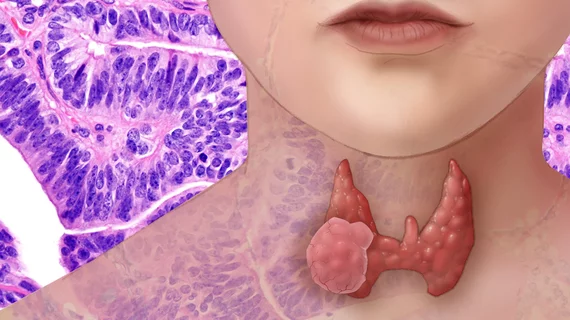
The use of such exams has increased each year in the U.S., expending unnecessary healthcare costs and leading to overdetection of clinically irrelevant nodules. Researchers with the University of Wisconsin School of Medicine and Public Health recently sought to better understand this trend, analyzing data from their own institution.
Of all 1,739 ultrasounds included in the study, one-fourth found a biopsy-recommended nodule, while 40% found no nodule at all, scientists detailed in the journal Thyroid [1].
“Providing clear guidance on when to order thyroid ultrasounds can help reduce unnecessary healthcare utilization and potential overtreatment,” Elena Kennedy, MD, a medical student in UW’s Department of Surgery at the time of the study, and colleagues concluded.
For the study, Kennedy et al. retrospectively analyzed all thyroid ultrasound performed between 2017 and 2019 at their academic center. The most common indications, they found, included suspected palpable nodule (40%), incidental imaging (28%), compressive symptoms (13%), combination (11%), metabolic symptoms (6%) and high-risk factors (2%). Overall, about 62% of ultrasounds found a nodule. Those performed for incidental findings had the highest rate of nodule detection at 94%, and compressive symptoms resulted in the fewest (39%).
Only about 27% of scans identified a biopsy-recommended nodule, while those found incidentally had the highest rate (55%). Compared with patients referred for a suspected palpable nodule, those with incidental ones were 10 times more likely to have a nodule found on an US.
Kennedy and co-authors believe this presents a prime opportunity to address healthcare waste and improve patient care.
“The number of thyroid ultrasounds performed in the United States has increased fivefold since 2002. This substantial increase produces a significant strain on healthcare resources and leads to over-detection and overtreatment of benign thyroid nodules and small, indolent cancers with questionable clinical relevance,” the authors noted.
Read more in Thyroid at the link below.