Over 134,000 US cancer cases went undiagnosed during COVID-19 pandemic’s peak
Over 134,000 U.S. cancer cases went undiagnosed during the peak of the COVID-19 pandemic, according to new data published Thursday in JAMA Oncology [1].
Cancers of the prostate (17%), female breast (13%), and lung (12%) accounted for the largest share of the tally, experts noted. Overall, screenable cancers saw a total rate reduction of nearly 14% during the time span between March and December 2020, compared to expected diagnosis rates.
University of Kentucky researchers believe these data offer key clues as radiology providers confront advanced cancer cases in the coming years.
“The U.S. experienced significant differences between observed and expected cancer incidence rates during the COVID-19 pandemic in 2020, with an associated and substantial deficit in diagnosed cases,” Todd Burus, with the Lexington-based institution’s Markey Cancer Center, and co-authors concluded. “The extent of differences varied based on cancer site, stage at diagnosis, and patient age and sex. These findings offer crucial information for current cancer prevention and control initiatives.”
For the study, UK researchers analyzed CDC cancer incidence data spanning 2018 to 2020. They used information from the time leading up to March 2020 to help forecast the expected number of cases the rest of that year after the pandemic declaration.
The study included nearly 1.3 million cancer cases reported in the U.S. between March and December 2020. Observed rates of all-site cancer incidence were about 29% lower than expected during the height of the COVID-19 response, Burus et al. noted. This included a roughly 6% shortfall between June and December or 13% lower during the first 10 months of the pandemic.
These percentages produced an overall estimate of 134,395 potentially undiagnosed occurrences of the disease. This included 22,950 instances of prostate cancer, 16,870 breast diagnoses, and 16,333 relating to the lung. Breast cancer diagnoses showed evidence of returning to pre-COVID levels after the first three months of the pandemic. But colorectal, cervical and lung cancers still lagged historic levels.
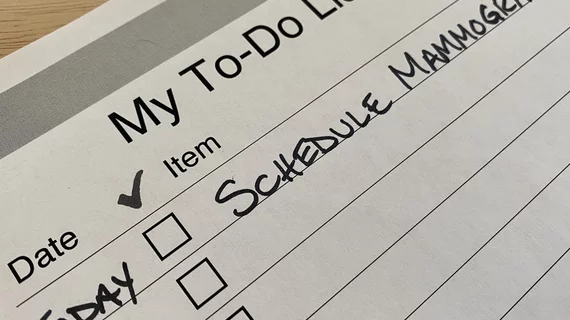
“Evidence of rate recovery for female breast cancer after the most restrictive pandemic response period suggests a resilience in mammography screening habits, likely borne from years of investment in public health messaging,” the authors noted. “It is important that we establish policies to help reengage with all patients regarding eligible screenings and necessary follow-ups, and work with patients to develop and maintain good cancer screening habits.”
Read more in JAMA at the link below.