Women do not need to delay their mammogram appointment after COVID-19 vaccination
Women do not need to delay their regular mammogram appointment after getting vaccinated against COVID-19, according to new research published Tuesday in Radiology.[1]
This concern first emerged in early 2021, with swollen lymph nodes (axillary adenopathy) appearing after inoculation posing diagnostic challenges for breast imagers. Such “unilateral lymphadenopathy,” affecting one side of the body, can also signal cancer and cause confusion during mammograms.
Experts at one point urged women to schedule annual breast exams around their shots to avoid potential false positives. But radiologists reported Feb. 8 that such vigilance is unnecessary.
“It is important for people to know that they should not delay their screening mammograms due to recent vaccination,” Stacey Wolfson, MD, with the Department of Radiology at New York University Grossman School of Medicine, Department of Radiology at NYU Langone Health in New York City, said in an RSNA announcement. “Reactive lymphadenopathy is common after COVID-19 vaccination — and benign.”
Wolfson and colleagues made their declaration after conducting a retrospective analysis of patients who received their vaccination and had breast imaging in the first few months of 2021. All told, the investigation included more than 1,200 individuals imaged across 17 NYU sites. Of those, about 44% (or 537 patients) experienced lymphadenopathy on at least one exam, the authors reported. Providers identified swelling on mammography alone in 9% of cases, ultrasound alone in 61%, and on both modalities at a 30% rate.
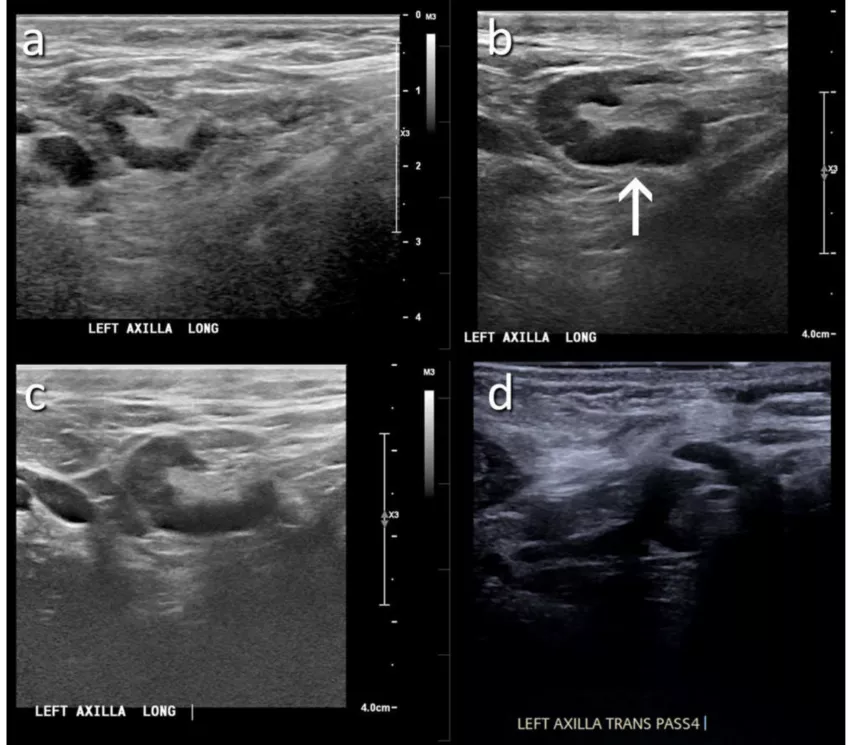
A 46-year-old patient with a strong family history of breast cancer had a screening ultrasound prior to COVID-19 vaccination demonstrating a morphologically normal left axillary lymph node. (B) 25 days following the second dose of the COVID-19 vaccination, the patient presented with a palpable lump in the left axilla and ultrasound demonstrated enlarged lymph nodes with cortex measuring up to 6 mm in thickness (arrow). (C) A follow-up ultrasound 21 weeks following demonstrated stable axillary lymphadenopathy. (D) An ultrasound-guided core biopsy was then recommended and pathology demonstrated lymphoid cells negative for carcinoma. Image courtesy of RSNA
Receiving the Moderna vaccine was significantly more associated with lymphadenopathy (46%) when compared to Pfizer (38%) or Johnson & Johnson (39%). Wolfson et al. found that patients developed swelling as early as one day after their first dose or as late as 71 days following the second shot. Persistent axillary lymphadenopathy (swelling occurring in the armpits) was found up to 43 weeks after vaccination. Out of the study population, only 9 cancerous lymph nodes were unearthed, in women with known cancer, concurrent suspicious findings in the breast, and/or contralateral axilla.
This is the largest study to date to evaluate this clinical concern and allows radiologists to establish broader guidelines dictating their response. Short-term follow-up imaging is not recommended, Wolfson emphasized.
“I was surprised by how quickly the lymph nodes became swollen and how long they persisted after being detected on routine screening mammogram and screening ultrasound exams," she said in a statement. "We found benign reactive lymph nodes were still present despite delaying the screening exams for 4 to 6 weeks based on various guidelines. These lymph nodes were unchanged with follow up exams at three months, and some enlarged lymph nodes persisted for over 10 months."
Read more in the Radiological Society of North America’s flagship journal here.
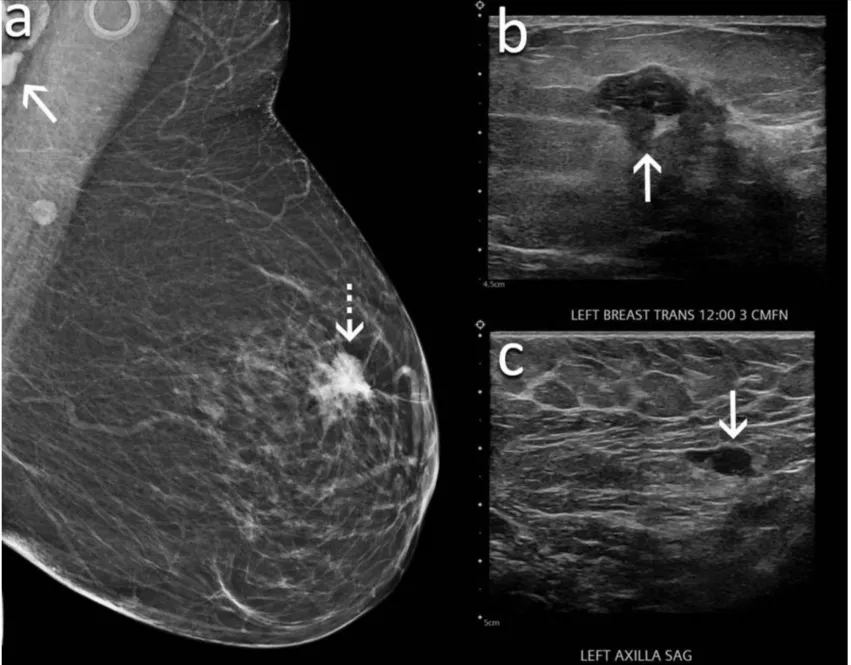
An example from the study of a 60-year-old woman presented for screening mammography nine weeks after receiving her second dose of the Moderna COVID-19 vaccine. (A) Mediolateral oblique view of the left breast demonstrates an irregular mass in the superior left breast (dash arrow) and a dense lymph node in the left axilla that is incompletely visualized (arrow). Sonography demonstrates (B) an irregular hypoechoic mass in the breast (arrow) that corresponded to the mammographic finding and (C) a lymph node with eccentric cortical thickening measuring 6 mm (arrow) in the axilla. Biopsy of the mass yielded invasive ductal carcinoma and biopsy of the lymph node yielded metastatic carcinoma. Image courtesy of RSNA
Related COVID vaccine-induced adenopathy in breast imaging:
VIDEO: Should women wait to get mammograms after COVID vaccination?
Women do not need to delay their mammogram appointment after COVID-19 vaccination.
Molecular imaging group shares updates for managing COVID-19 vaccine effects on PET/CT exams
How radiology providers can minimize mammography recalls among COVID-vaccinated patients
Most routine imaging should be scheduled 6 weeks after 2nd vaccine dose, major cancer centers say
Managing COVID-19 vaccine side effects: Harvard radiologists share their ‘pragmatic’ approach
COVID-19 vaccine update: Radiologists report side effects mimicking breast cancer on mammograms
Radiologists report COVID vaccine side effects mimicking breast cancer on mammograms
These ultrasound features distinguish between COVID vaccine-related and malignant adenopathy
Reference: