A Physician, a Patient and a Technology Whose Time Is Now
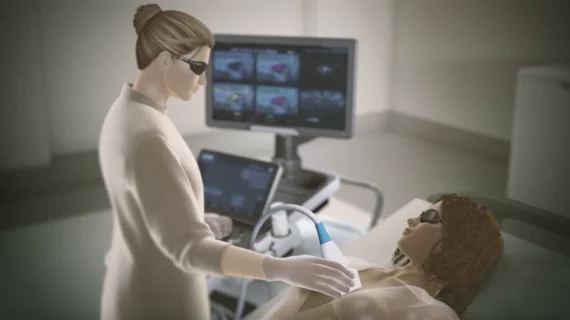
If certainty is the holy grail of diagnostic breast imaging, then opto-acoustic ultrasound is the treasure map showing exactly where to find it. While other imaging modalities can help distinguish a benign lesion from a malignant mass, only OA/US provides the radiologist with a more definitive diagnosis without invasive medicine, ionizing radiation or claustrophobic dread.
And that happens the first time it’s tapped to shed literal light—the laser kind—on a patient’s worrisome screening: It’s a one-and-done imaging exam with Seno Medical’s Imagio® OA/US Imaging System.
Thomas Stavros, MD, reminded Radiology Business of this distinction in a recent interview. In doing so, he pointed to objective scientific data painting the creative word picture above.
“Breast imagers appropriately view the cost of a false negative to be much higher than the cost of a false positive, and thus they demand a sensitivity of 98% or better to arrive at a confident call on whether or not to biopsy,” he says, citing a 2018 study that helped prompt the FDA to approve Imagio® as the first OA/US system for U.S. markets in 2021. [1] “Unfortunately, such high sensitivity comes at the cost of a low specificity, resulting in lots of false positives and lots of biopsies of benign masses.”
Stavros, Seno’s CMO, is a well-known breast specialist. He already had 30 years of experience in clinical care, research and teaching when he joined the company in 2012.
He points to Imagio’s® differentiators to underscore the confidence seen regarding specificity and sensitivity. OA/US post-approval studies shows the system’s specificity ranged from 64% to 74% with sensitivity of 98.5% to 100%. [2,3]

‘Sure, breast MRI is the best screening test. It’s also the best for cancer staging. But opto-acoustics can beat it in diagnosis.’
Tom Stavros, MD, Chief Medical Officer, Seno Medical
By comparison, breast MRI—long considered the “gold standard”—had specificity of just 50% at a sensitivity of 98.1%. [4]
“For adjunctive diagnosis of breast masses, we beat MRI in both sensitivity and specificity,” Stavros underscores, acknowledging that Imagio® had Seno’s AI toolkit, SenoGram®, in its corner. “Sure, breast MRI is the best screening test. It’s also the best for cancer staging. But opto-acoustics can beat it in diagnosis.”
Contrast-enhanced spectral mammography has similarly failed to equal OA/US at overall accuracy or predictive value. [5] Plus it’s primarily indicated for supplemental screening of dense tissue and neoadjuvant monitoring of breast cancer. Besides, Stavros adds, contrast is generally best avoided unless it’s truly necessary.
“I’m a true believer in opto-acoustic breast imaging,” Stavros says. “Anyone who reviews the research on this technology will find the data incontrovertible.”
The evidence supporting OA/US as the “best first” diagnostic test for noncalcified breast masses found in screening, he adds, is “as strong as anything I’ve ever seen in diagnostic radiology.”
Informed patient, astute observations
Stavros is not alone among cancer experts voicing high confidence in opto-acoustic breast imaging. In 2024, some of the technology’s most outspoken champions are knowledgeable patients.
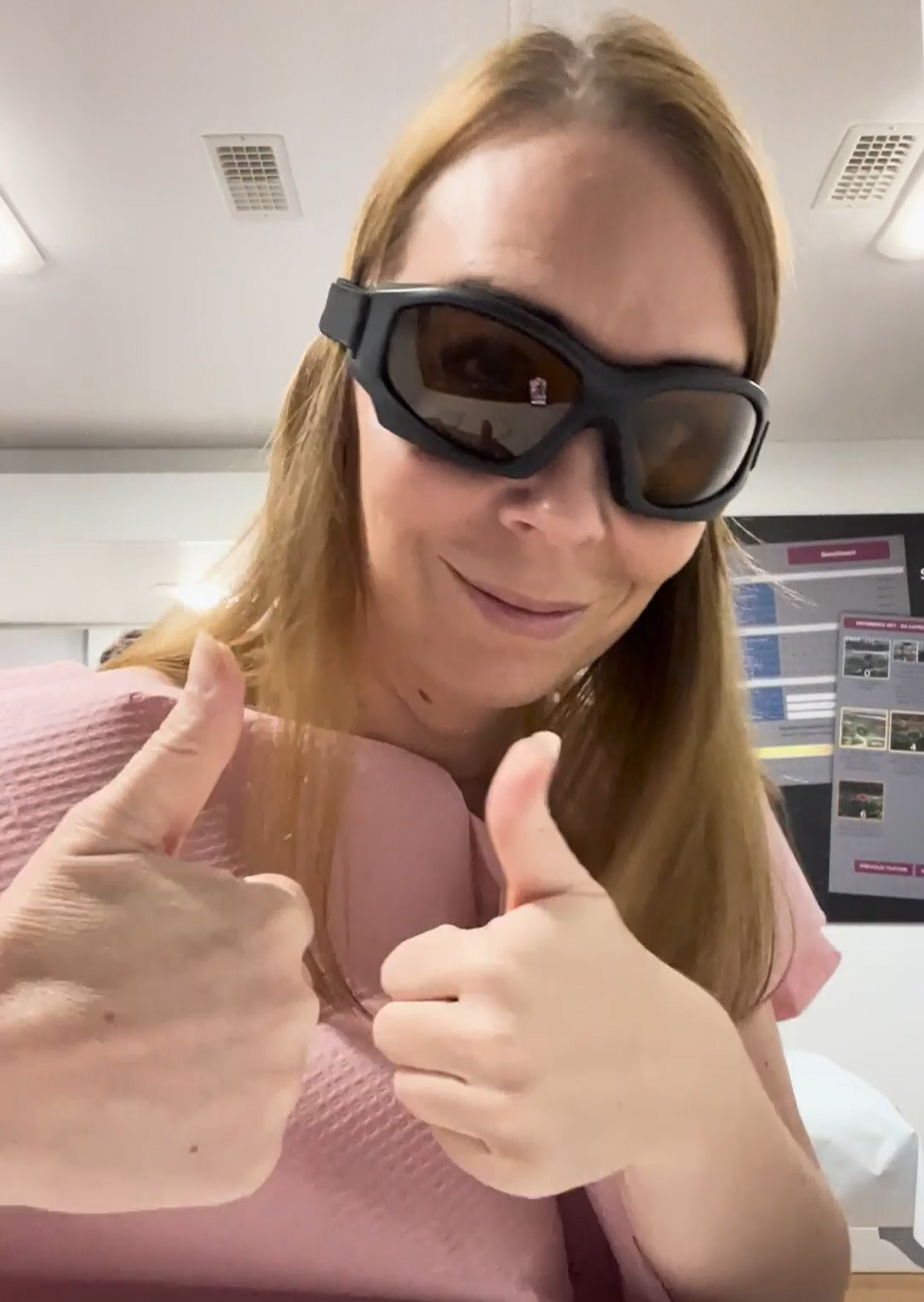
Corrine Ellsworth-Beaumont, MFA, PhD, is one. After discovering a lump five years ago, the award-winning graphic designer received a mammogram and a supplementary ultrasound. This was ordered due to dense breast tissue. Upon reviewing the results, the care team said the lesion was probably a fibroadenoma. This is a common, noncancerous breast lump that presents as a solid lump. It tends to cause no pain and can take any number of shapes.
“It really felt like they were making a lot of assumptions rather than looking at data,” recalls Ellsworth-Beaumont, whose doctorate is in design thinking for healthcare.
She based her distrust on three primary factors. One, she had some pain. Two, she was older than most women who get fibroadenomas. And three, the advice she received—
“Come back every six months to have your lump checked and maybe re-imaged”— seemed overly passive.
“I had the sense,” she says, “that they were relying too much on guesswork.”
Be gone, biopsy
This didn’t sit well with Ellsworth-Beaumont, and it’s easy to understand why. In prior years, she’d lost both grandmothers as well as a lifelong friend to breast cancer. These experiences had made her an energetic breast-health advocate: She’s the force behind the nonprofit “Know Your Lemons” breast-health campaign and foundation. This campaign went viral in 2017 and has educated more than 2 billion people speaking 40 or so languages across almost 100 countries.
With her own breast health on the line, Ellsworth-Beaumont eventually turned to Seno Medical, with which she was somewhat familiar through her advocacy work. After getting imaged with Imagio® in 2023, she discussed her findings with the radiologist reading her OA images.
“He said my lump was likely not a fibroadenoma and exhibited OA characteristics similar to a papilloma,” she remembers. This diagnosis explained the pain she’d been feeling at the site of the lump. It also justified the active role she was now taking in her own care, since papillomas do bring some risk of breast cancer.
“It was really helpful to get that information without having to get a biopsy,” says Ellsworth-Beaumont, who served on a working group of the World Health Organization’s Global Breast Cancer Initiative.
She especially appreciates the insights supplied by OA/US’s unique ability to show how a lesion is behaving on top of what it looks like.
“Of course, the lump still has to be monitored,” she says. “But since it hasn’t changed over the five years since I first discovered it, the chances of it becoming cancerous are very low. The confidence I feel in the diagnosis made with OA/US has taken a lot of worry off my mind.”
‘The right technology at the right time’
At this point in her breast-health journey, Ellsworth-Beaumont conveys, her drive is as strong as ever to preach early detection for women around the world—and to explain OA/US to breast-health professionals wherever she can reach them.

‘I’m really looking forward to the day when this technology is better known and appreciated.’
Corrine Ellsworth-Beaumont, MFA, PhD, Founder and CEO, Know Your Lemons Foundation & Dandelion Health
“I’m really looking forward to the day when this technology is better known and appreciated,” she says. “It’s just one piece of the puzzle—but for those with access to it, OA/US can be the piece that makes a major difference in their lives.”
“At the same time,” she adds after pausing to gather her thoughts, “we can have all the tools and technologies and treatments in the world. But if people aren’t educated—if they aren’t reporting symptoms, if they aren’t getting screened—we will always be stuck with the problem of far too many people dying from breast cancer.”
Stavros amplifies the observation.
“The greatest benefit breast imagers can offer to society is to maximize screening exams while minimizing diagnostic examinations and negative biopsies and cutting out the need for second—or third or fourth—diagnostic exams,” he says. “That’s especially true today, given the worsening shortage of breast specialists to timely read all those exams. Opto-acoustic imaging can help our profession meet these challenges. It’s the right technology at the right time.”
For more:
References:
- Vlahiotis A, Griffin B, Stavros AT, Margolis J. Analysis of Utilization Patterns and Associated Costs of the Breast Imaging and Diagnostic Procedures After Screening Mammography. ClinicoEconomics and Outcomes Research, 2018:10 157-167.
- Ghannam S, Koneru V, Karabon P, Darling R, Kist K, Otto P, Van T. Exploring the Utility of Optoacoustic Imaging in Differentiation of Benign and Malignant Breast Masses: Gen 2 Study. Academic Radiology, 2024 October.
- CONFIDENCE Registry Study (Netherlands). ClinicalTrials.Gov NCT05084729
- Milon A, Flament V, Gueniche Y, Kermarrec E, Chabbert-Buffet N, Darai E, Touboul C, Razakamanantsoa L, Thomassin-Naggara I. How to optimize breast MRI protocol? The value of combined analysis of ultrafast and diffusion-weighted MRI sequences. Diagnostic and Interventional Imaging, 2023 Jun;104(6):284-291.
- Gelardi F, Ragaini EM, Sollini M, Bernardi D, Chiti A. Contrast-Enhanced Mammography versus Breast Magnetic Resonance Imaging: A Systematic Review and Meta-Analysis. Diagnostics (Basel, Switzerland), 2022 Aug 4;12(8):1890.