Researchers urge nonradiologists to stay in their lane when interpreting advanced imaging studies
Nonradiologist physicians do not receive enough formal training to warrant allowing them to interpret complex imaging studies.
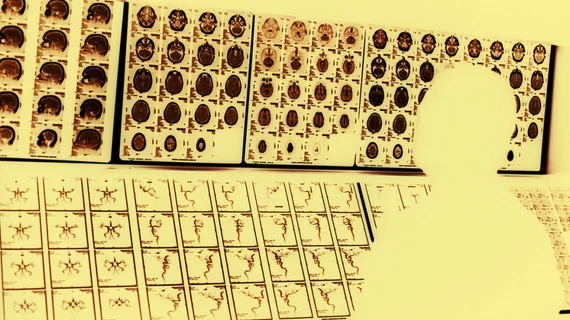
That’s one of the key takeaways from a new study by Thomas Jefferson University Department of Radiology researchers, published Nov. 6 in the American Journal of Roentgenology. Poring over 2015 Medicare data from millions of CT, MRI, PET and general nuclear imaging tests, Kofi-Buaku Atsina and colleagues found that radiologists did, in fact, perform the vast majority of interpretations. But nonradiologists are still interpreting thousands of tests, presenting the quandary of whether policy changes are needed to help preserve patient safety and continuity of care.
“Aside from cardiologists, no other medical specialty provides sufficient education for their trainees in advanced imaging to justify allowing them to interpret these studies in practice, except under carefully controlled circumstances,” Atsina and colleagues wrote.
According to their analysis, nonradiologists interpreted about 126,000 (or 0.71%) of all CT scans in the Medicare fee-for-service population, compared to almost 17.7 million for radiologists. Numbers were similarly skewed for MRI exams (about 43,000 or 0.96% interpreted by non-radiologists) and PET scans (23,000 or 5.8%). Meanwhile, nonradiologist doctors interpreted about 760,000 (or 37%) of general nuclear medicine studies, according to the analysis of data from the CMS Physician/Supplier Procedure Summary Master Files.
Cardiologists accounted for the largest proportion, interpreting about 3% of all advanced imaging studies in 2015, with other physicians accounting for a “tiny fraction.”
The American College of Radiology’s Practice Parameters stipulate that nonradiologist physicians who intend to interpret CT or MRI scans should have read 500 of these studies in a supervised setting first, among other things. However, with so few of such studies interpreted by non-expert physicians in hospitals, these physicians “have limited (if any) opportunities to achieve the required 500 interpretations,” Atsina and colleagues wrote.
Also, radiology residency requires a minimum of 48 months of intense education. On the flipside, other residency programs “do not offer sufficient education in diagnostic imaging and depend heavily on short rotations through the radiology department, during which the resident is passively observing as opposed to actively involved, and proper imaging education is inconsistent.”
The authors conclude by arguing that policy levers may need to be pulled to ensure that advanced imaging studies are only interpreted by experts. As one example, commercial payers in Connecticut, Massachusetts, Pennsylvania and New Jersey have explored policies that restrict imaging privileges for clinicians who are not radiologists.
“If a hospital credentialing committee is too lax, or it grants privileges simply to entice physicians to admit their patients (so-called economic credentialing), inadequate imaging interpretation can result,” they concluded.