Radiologists must fight ‘disturbing’ efforts to limit positive oral contrast use in CT
A Wisconsin-based gastrointestinal imaging expert is urging radiologists to carefully consider whether they should use positive oral contrast materials in abdominal CT care. And at the very least, he wants his peers to avoid kowtowing to nonradiologists in this important decision.
The University of Wisconsin’s Perry J. Pickhardt, MD, made his pitch in a new analysis, published Jan. 8 in the American Journal of Roentgenology. He’s motivated by the “disturbing recent trend” of emergency department doctors, surgeons and even hospital administrators influencing such care-level decisions for the sake of expediency and financial reasons, without considering its impact to patient care. Use of such materials often add about 30 to 40 minutes to turnaround time, he noted.
Pickhardt said that there’s been some debate about whether positive oral contrast can genuinely improve diagnostic confidence. However, he’s convinced that it does, and believes “it behooves us to keep fighting for its use.”
“As radiologists, we owe it to our patients to drive the appropriate use of positive oral contrast material,” wrote Pickhardt, chief of gastrointestinal imaging at the University of Wisconsin School of Medicine and Public Health. “At the very least, we should not allow nonradiologists to restrict its use solely on the basis of throughput concerns; rather, we should allow considerations of image quality and diagnostic confidence to enter into the decision process.”
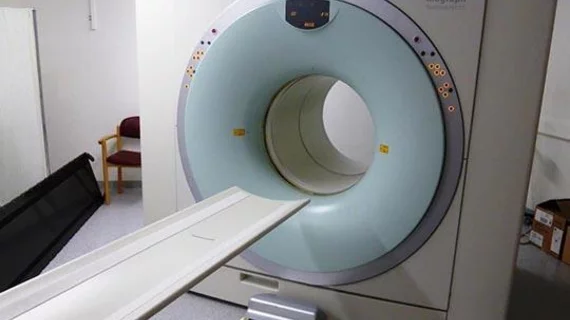
Radiologists’ use of such contrast materials dates back to the earliest days of CT scans. With evolving technology and imaging methods, however, there has been wide variation among practices in their deployment, with some physicians labeling them “old fashioned” and others still using such materials for a wide variety of indications, Pickhardt wrote.
The author runs through some of the past studies on this topic, but argues that the existing medical literature on this controversy is “largely devoid of properly designed and powered studies to fairly and adequately address the key questions.” Furthermore, he believes there is a degree of subjectivity as measuring the clinical value of positive oral contrast materials is difficult.
Bottom line, Pickhardt concludes that decisions on whether to use such materials in everyday abdominal CT imaging should be made on a case-by-case basis, and by individuals with training in radiological care.
“There is often no simple answer, but indication-specific considerations should generally hold sway,” he wrote. “Oral contrast material (whether positive or neutral) can reduce diagnostic error and can increase diagnostic confidence. I believe that there is definitely still a role for positive oral contrast material in modern state-of-the-art abdominal CT.”