Imaging-based COVID study finds blood clots twice as likely with infection vs. vaccination
Early on in the COVID-19 pandemic, fears over stroke due to vaccine-induced blood clotting led to a 40% spike in orders for vein imaging with both CT and MR at an academic medical center in the Eastern U.S.
However, a retrospective analysis shows only 4.5% of the institution’s vaccinated patients had a clotting condition while the rate for the unvaccinated was 10.1%.
The research is described in a study published online July 14 in Clinical Imaging [1].
Corresponding author Ana Franceschi, MD, of Northwell Health in New York and colleagues reviewed venograms performed at a single hospital prior to and during the pandemic.
Focusing on cross-sectional exams, which combine MR and CT views, the team found 321 scans completed in the first four months of 2021. Had the hospital maintained that pace for the whole of that year, it would have performed more than 960 such exams.
By comparison, the full-year totals from 2018, 2019 and 2020 were, respectively, 568, 657 and 660.
Other key findings from the review:
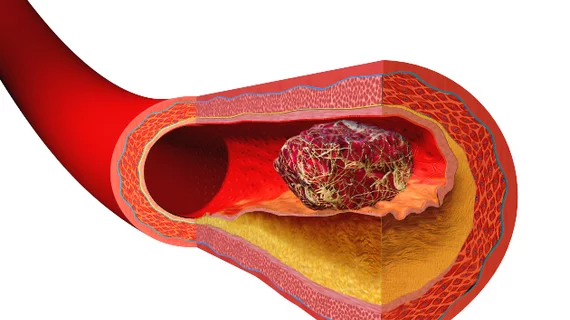
- Where present, vaccine-induced immune clotting conditions—predominantly thrombotic thrombocytopenia (TT) and cerebral venous sinus thrombosis (CVT)—were mainly associated with adenovirus viral vector vaccines such as those from Oxford-AstraZeneca and Johnson & Johnson.
- Vaccine-induced TT and CVT symptoms occurred five to 30 days post-vaccination. Headache was the single most common symptom.
- Both CT venography and MR venography were helpful in arriving at a confident diagnosis.
In their discussion, Franceschi and co-authors encourage trust in COVID-19 vaccines:
Patients with COVID-19 compared to unaffected populations have a 30 to 60 times increased risk of cerebral venous thrombosis, and up to a third of patients with severe COVID may have thrombotic complications. Currently, vaccination is the best countermeasure in preventing severe COVID-19.”
Tracing the timeline of developments relative to the review, the authors point out that, prior to the start of the pandemic, CTV accounted for just 0.5% of all strokes.
Meanwhile, as cautionary measures grew along with public avoidance of care sites during late 2020 and early 2021, cross-sectional venography volumes initially fell. That changed quickly.
“In early 2021, reports of adenoviral vector COVID vaccines causing cerebral venous thrombosis and thrombotic thrombocytopenia led to a 39.65% increase in cross-sectional venography,” the authors underscore. “[H]owever, in this study, unvaccinated patients in 2021 had higher incidence of CVT (10.1%), compared to the vaccinated patients (4.5%).”
More:
Clinicians should be aware that vaccine-induced thrombotic thrombocytopenia and cerebral venous sinus thrombosis may present with a headache five to 30 days post-vaccination with thrombosis best diagnosed on CT venography or MR venography. If thrombosis is present with thrombocytopenia, platelets <150 × 109, elevated D-Dimer >4000 FEU, and positive anti-PF4 ELISA assay, the diagnosis is definitive.”
The study is available in full for free.