Management
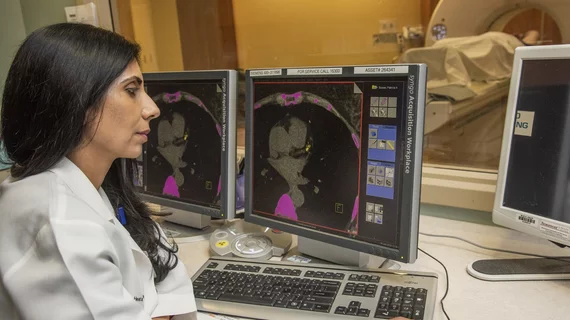
This page includes content on healthcare management, including health system, hospital, department and clinic business management and administration. Areas of focus are on cardiology and radiology department business administration. Subcategories covered in this section include healthcare economics, reimbursement, leadership, mergers and acquisitions, policy and regulations, practice management, quality, staffing, and supply chain.
Displaying 7801 - 7808 of 9989