Beyond Scanning and Beaming: ‘Techs’ Are Well-Organized Advocates Too

As the lead advocacy organization for the medical imaging and radiation therapy profession, the American Society of Radiologic Technologists (ASRT) is dedicated in its mission to advance the profession and enhance patient care. For us, protecting patient safety, advancing healthcare standards and guiding smart policy are fundamental priorities.
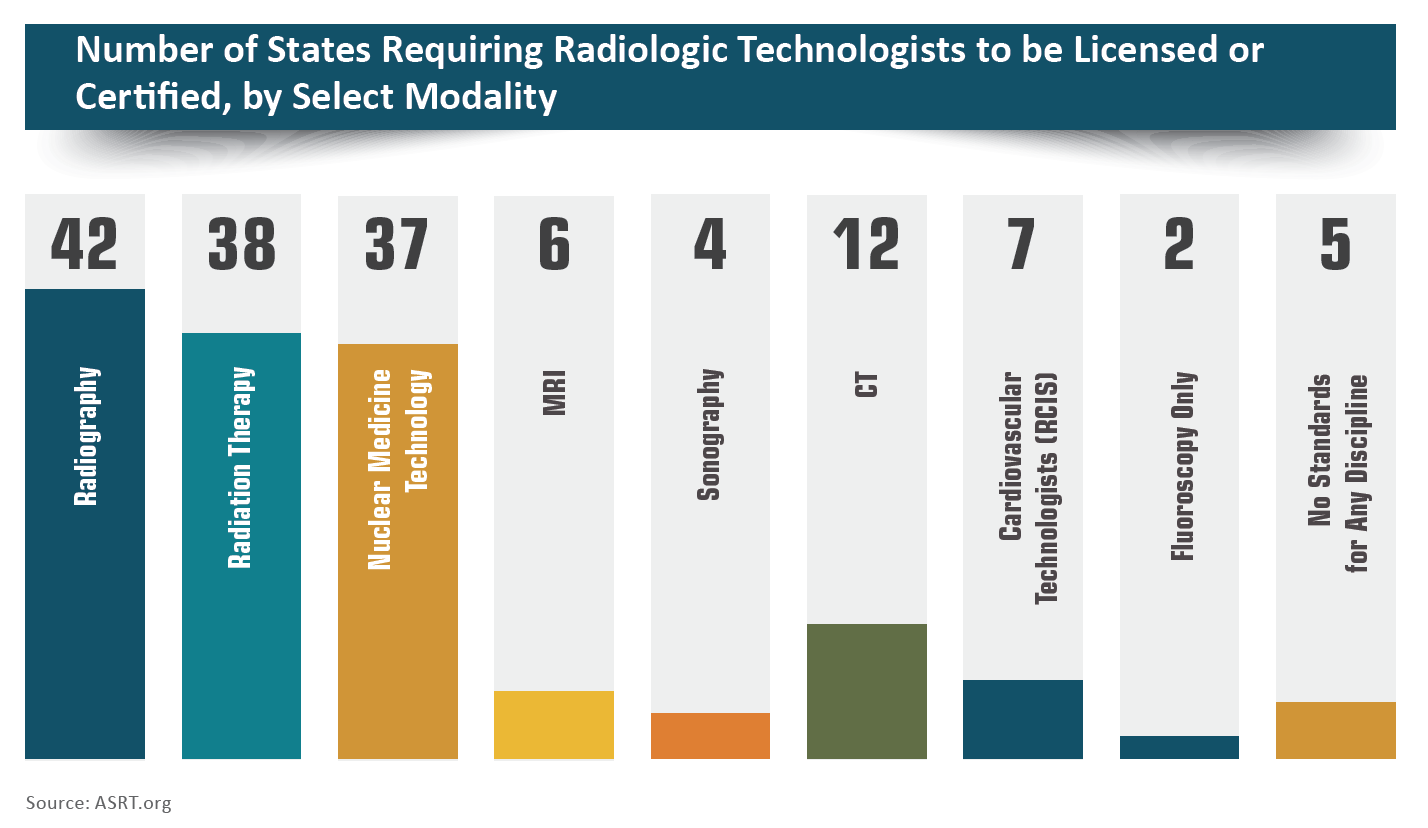
Outside of our profession, not everyone knows that there is no single federal requirement for the licensing of radiologic technologists. Licensing is left to state control. Unfortunately, many states still have no minimum education and credentialing standards for those who perform medical imaging exams and radiation therapy treatments.
In 2014, ASRT shifted its focus away from legislation at the federal level and instead began concentrating our licensure advocacy efforts on the state level. Here’s why: In 1981, Congress passed the Consumer Patient Radiation Health and Safety Act, which directed the Secretary of Health and Human Services within each state to establish a process for licensing anyone who administered ionizing or non-ionizing radiation for both medical and dental procedures. In the end, the standards were adopted, but following them became a discretionary decision for the states. No sanctions were included for compliance.
In the pursuit of improved patient safety, ASRT has always been committed to upholding those standards. However, there have been challenges at the state level. Today in the United States, we have an uneven patchwork of laws and regulations that vary widely from state to state. Some states regulate the medical imaging equipment that produces ionizing radiation but have no standards for the professionals who operate them. Some states regulate only certain modalities. Others may regulate by the type of facility in which an exam or procedure is performed. Then are the states with no regulations at all. To understand how your state regulates radiologic technologists, go to ASRT.org > Standards & Regulations > Legislation, Regulations and Advocacy.
There are other pressures on licensure, too. Under what’s sometimes called occupational license reform, states with long-held and successful licensure standards today face a national wave of occupational deregulation that seeks to eliminate it for many professions, including medical imaging and radiation therapy. That kind of change may be advisable for some occupations, but if states decide to abolish licensure for radiologic technologists, patients may be put in serious potential danger.
What’s alarming is that legislatures in numerous states—including Arizona, Florida, Indiana, Kentucky, Louisiana, Massachusetts, Mississippi, Missouri, Nebraska, New York, Ohio, Utah, Washington and Wyoming—saw occupational deregulation bills introduced in 2018. We worked closely with our state affi liate societies to oppose many of these measures, but we expect to see more occupational deregulation bills introduced this year and in the future.
In addition to deregulation efforts, we also stand against encroachment or “scope creep.” When other allied health professionals lobby to be exempt from regulations requiring strict educational and certification standards to carry out medical imaging or radiation therapy procedures, we oppose those measures. Our aim is always to ensure patient safety.
For example, in 2016 the U.S. Department of Veterans Affairs floated a proposal that would allow nurse practitioners to order, perform and interpret diagnostic imaging procedures. While the intent was to increase access for veterans, the proposal’s leaders didn’t calculate the risks. ASRT, our affiliates and the public sent them thousands of letters explaining that our veterans and families deserve the highest quality care. The VA heard our concerns and removed the language from the regulations.
Making sure educated and qualified professionals perform procedures is crucial for patients. Medical imaging and radiation therapy personnel take specialized courses in anatomy, positioning, radiation safety, radiation physics and exposure techniques to be able to create an image that contains the data radiologists need to diagnose patients.
For instance, an individual who isn’t trained in exposure techniques for something as simple as a chest X-ray could under- or over-expose the image. Then it wouldn’t contain the detail a radiologist needs to see the pathology or identify what needs to be diagnosed. This could result in missed diagnoses or repeated exposure to ionizing radiation for subsequent exams. It’s critical that those performing medical imaging exams or radiation therapy procedures meet education and certification licensure standards and demonstrate their clinical competency.
ASRT is always in the mix to educate lawmakers and the public about the importance of having certified and registered radiologic technologists on the job. It’s the best way to ensure that patients receive safe, high-quality care. We’re committed to advocating for comprehensive state licensure requirements, and we encourage the radiologic technology community to join us in our efforts.
Melissa Jackowski is president of the American Society of Radiologic Technologists (ASRT).
