MedPAC Wants MIPS to Go Away. Should the Group Get Its Way?
We are now firmly in the era of the MACRA legislation that abolished the sustainable growth rate formula and created a “new” methodology for physician reimbursement. As a quick review, MACRA created the Quality Payment Program (QPP) with two distinct payment tracks:
- MIPS, or the Merit-based Incentive Payment System. This track bases physician reimbursement on four pillars—cost, quality, interoperability and improvement activities. Individual physicians or groups of physicians are evaluated on each of these pillars and compared to a performance threshold. The comparison determines whether CMS pays a bonus or assesses a penalty.
- Advanced Alternative Payment Model (APM). This track requires networks to assume financial risk for their patients, the hope being that this will incentivize facilities to provide high-quality, high-value care. APMs can apply to a specific clinical condition, a care episode or a population.
Underlying both arms of the QPP is Medicare’s intention to drive up the value of healthcare by increasing quality while decreasing costs. That’s certainly a worthwhile goal, but not everyone is convinced that MIPS can help achieve it.
In fact, the powerful independent congressional agency known as MedPAC, the Medicare Payment Advisory Commission, has recommended that MIPS be scrapped.
You read that right.
This influential agency advocates the complete dismantling of a payment system that took years to develop—and that cost providers an estimated $1.3 billion in its first year of implantation alone.
MedPAC’s 17 members did not come to this recommendation on a whim. In the 21-page section of the advisory group’s report devoted to this topic released in March, they elaborate on the multiple reasons for this recommendation. For example, they discuss the possible gaming that can occur due to the flexibility the system offers around picking measures. This could shift providers’ focus, MedPAC notes, from improving quality to maximizing reimbursement.
They’re correct, of course. In addition, an unequal basis of comparison is inherent in the flexibility to choose measures. This could negate the principle of the performance threshold, which aims to reward or penalize clinicians based on how others are performing.
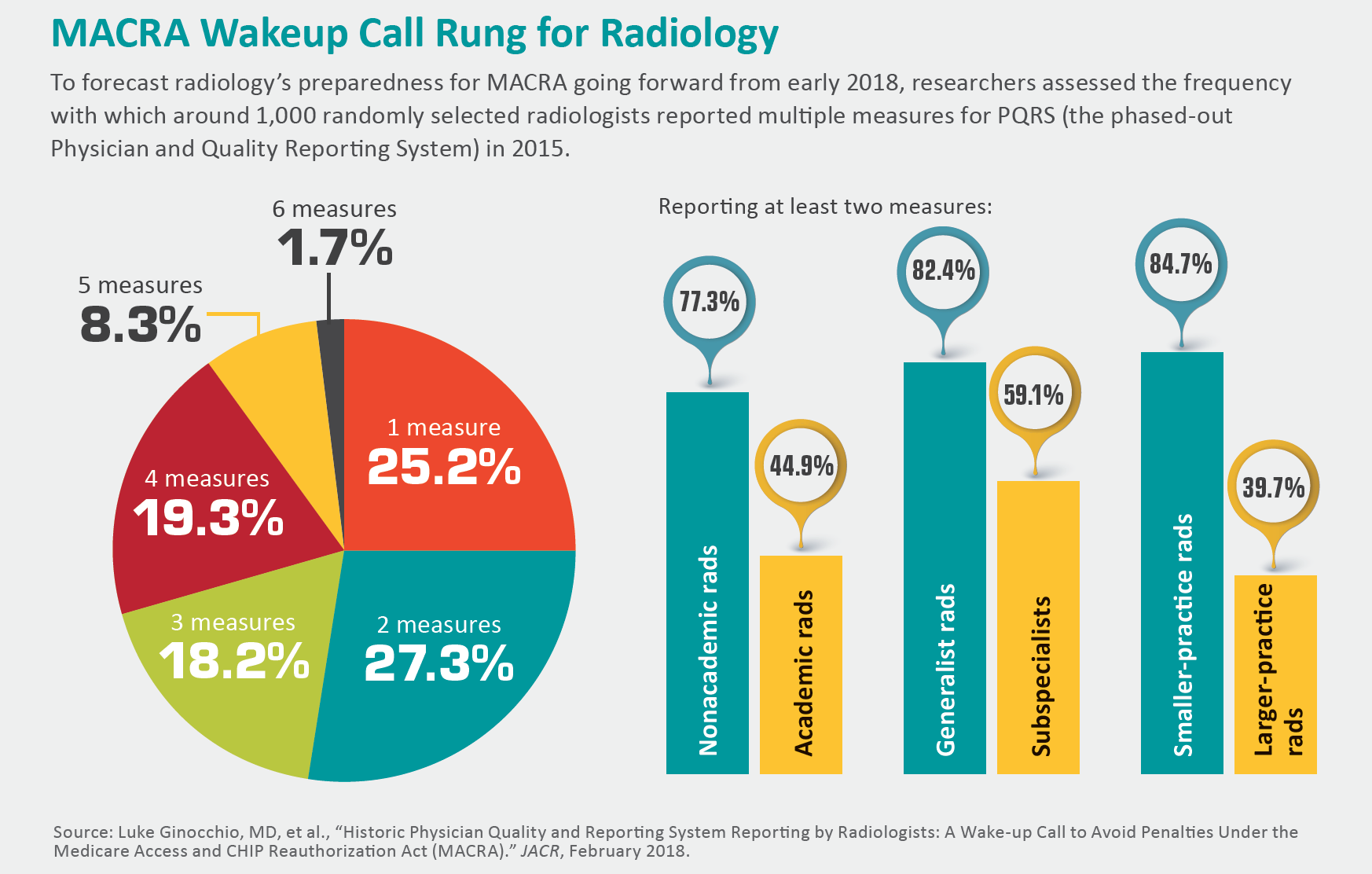
What’s more, MIPS is largely based on preexisting programs—PQRS, Meaningful Use, Value Modifier—that have not been shown to actually improve the quality of care.
Finally, considering the extensive cost and time burden of implementing MIPS, the incentives in the early years are minimal. This creates significant uncertainty for networks down the line (even though the plan is for larger incentives in later years).
MedPAC doesn’t just critique MIPS. They also present an alternative plan. Well, sort of.
MedPAC references development of a voluntary value program (VVP) in which clinicians would be measured under the same measures in groups that they could organize themselves into. Unfortunately, specific details for how this program would work are lacking. And as we all know, the devil is in the details.
Part of the rationale for this alternative VVP is that it would allow clinicians to become facile with the concept of an alternative payment model, providing an easier transi-tion. Then too, this is exactly the rationale behind MIPS as well.
Much has been written on the deficiencies of MIPS, and MedPAC is not the only organization to criticize it. However, are the deficiencies of MIPS significant enough to warrant a complete abandonment now that clinicians and networks have sunk big dollars into its participation? Much has been spent on consultation fees, programs and administrators specifically to deal with the rigorous demands of successful participation in MIPS.
On the other hand, it is exactly the complexity of this program that has many frustrated with it, and an extensive overhaul that simplifies and streamlines the program would certainly have benefits. It is difficult to educate clinicians on how to successfully participate in this very complicated program.
I can say from personal experience that explaining even one pillar of MIPS can be a challenge. For example, “promoting interoperability” (formerly “advancing care information”) is a difficult topic, as this pillar encompasses multiple individual measures that can have complex numerators and denominators. The quality pillar can be similarly difficult to educate clinicians on, and we have not even begun to discuss how the cost pillar is calculated or how to choose an improvement activity in which to attest.
Many clinicians with whom I have interacted see MIPS as yet another burdensome task that has been assigned to them with no obvious benefit. This perception needs to change if a greater amount of buy-in from participating clinicians is to be achieved.
CMS has begun rolling out programs designed specifically for this purpose. However, these programs have so far reached very few clinicians. Enlarging and robustly advertising these programs would go a long way toward pushing along physician education and acceptance of MIPS.
The recent proposed rule for QPP in its third year suggests that CMS has no intention of acting on MedPAC’s recommendation anytime soon. The current proposed rule has relatively modest changes. Still, as is always the case, we will have to wait with bated breath for what the final rule will bring.
Dr. Lee is a clinical associate professor at Thomas Jefferson University and section chief of neuroradiology at Philadelphia-based Einstein Healthcare Network.